FUTURE Content Hub
An archive of key moments so you can experience the 2025 conference.

The FUTURE of medicine specialty in motion
At FUTURE 2025, sessions were full and conversations were flowing. For three days, family medicine was the focus for more than 1,500 med students and residents. The FUTURE Content Hub replays great moments and introduces you to members who played an important role in supporting the next generation of physicians.
We selected a few sessions each day and created quick takeaways in case you couldn’t make it!
Creating a Life You Love as a Doctor in Training
Why This Topic Matters to Family Medicine
Dr. Marc Levin’s presentation addresses a critical challenge in family medicine: physician burnout and the need for sustainable, fulfilling careers. With 27 years of experience across diverse settings—from war zones with Doctors Without Borders to remote Alaska villages—Dr. Levin offers a perspective on aligning medical practice with personal values and well-being.
Family medicine students who will face unprecedented career pressures and need tools to create meaningful, sustainable practices while serving patients effectively.
Five Key Takeaways for Medical Students and Residents
- Commit to Yourself First: "The first thing you need to commit to before you commit to anyone else, is yourself." Self-advocacy and boundary-setting aren't selfish—they're essential for sustainable patient care.
- Define Your Mission Statement: Create a two-part personal mission that includes both what serves you and what serves others. This prevents burnout by ensuring you're nurtured while giving.
- Embrace Non-Traditional Paths: Family medicine offers unlimited possibilities beyond academic medicine. Dr. Levin works only 18 weeks per year while maintaining a full salary through creative practice arrangements.
- Focus on Your Highest Expression: "Your only job is to continually achieve your highest expression of self." Every career choice should move you toward becoming more authentically yourself.
- Transform Your Relationship with Pain: "The wisest ones invite pain in and say sit down and don't leave until you’ve taught me what I need to know." Growth comes through facing challenges, not avoiding them.
"My job is just to light up my little corner of the world, wherever it is, the way that only I can." – Dr. Marc Levin

The Insider's Guide to Making the Most of Medical School
Why This Topic Matters to Family Medicine
This dynamic panel brought together medical students, residents and attending physicians to share authentic insights about navigating medical training successfully. The diverse perspectives—from current students still in the trenches to seasoned faculty who've weathered the journey—provided invaluable wisdom for family medicine students and residents who value holistic care, work-life balance and genuine patient connections.
The panel's emphasis on maintaining authentic identity while developing professional competence directly aligns with family medicine's core values of treating the whole person. As one panelist noted, "We should give ourselves that same holistic view we give our patients—accepting all the things that make us who we are."
Five Key Takeaways for Medical Students and Residents
- Embrace Vulnerability as Strength: "Don't be afraid to say 'I've never done this before. Can you please help me?' Letting go of trying to be perfect and being willing to learn from everyone around you—nurses, residents, attendings—is crucial for growth."
- Develop Self-Directed Learning Early: Take initiative in your education rather than waiting to be taught everything. "There's a lot of self-directed learning in medicine, and I wish I had known that sooner."
- Maintain Your Authentic Identity: Professional development doesn't require abandoning who you are. "In addition to being a very type A medical student, I also love to have days with no schedule and travel and backpack—things that have nothing to do with medicine."
- Prioritize Mental Health: "Getting involved with my school's therapy services made such a difference. Talking to someone who really understands. I'm better at exams now because I can think more clearly and remember what my real goals are."
- Stay Present and Engaged: "Be more present in the moment and really soak in what's happening on rotations. Learn something from everyone, whether you're interested in that rotation or not."
Financial Literacy for Family Medicine Students
Why This Topic Matters to Family Medicine
Financial literacy is crucial for family medicine students who face unique challenges including extended training periods, delayed income, and substantial debt loads. As the presenter noted, "physicians have a really odd trajectory frame" - going from college to medical school to residency with "tons of loans while the rest of our peers are earning." This financial education session addresses the strong correlation between financial well-being and overall resident well-being.
Family medicine physicians will earn an average salary of $272,000, placing them in the top 5% of income earners. But the path to financial stability requires strategic planning during the critical period of late medical school through early attending years, which "are the best sort of predictors for how you're going to be long term."
Five Key Takeaways for Medical Students and Residents
- Pay Yourself First: Start financial planning with savings and investments rather than expenses. "You're going to start thinking about your financial planning with your savings and investments."
- Follow the 50/30/20 Rule: Allocate 50% of income to fixed expenses, 30% to discretionary spending and 20% to wealth building through debt repayment and savings.
- Maximize Your Employer Match: "That is free money, and you should really try to get it" through retirement account matching programs, even during residency.
- Consider PSLF Strategically: Public Service Loan Forgiveness can benefit those planning nonprofit careers but requires careful documentation and understanding of new income-based repayment plans.
- Start Investing Early: Even small contributions during residency benefit from compound interest over time, making early investment crucial for long-term wealth building.
"There's a really, really strong correlation between financial well-being and overall resident well-being." – Dr. Stacy Bartlett
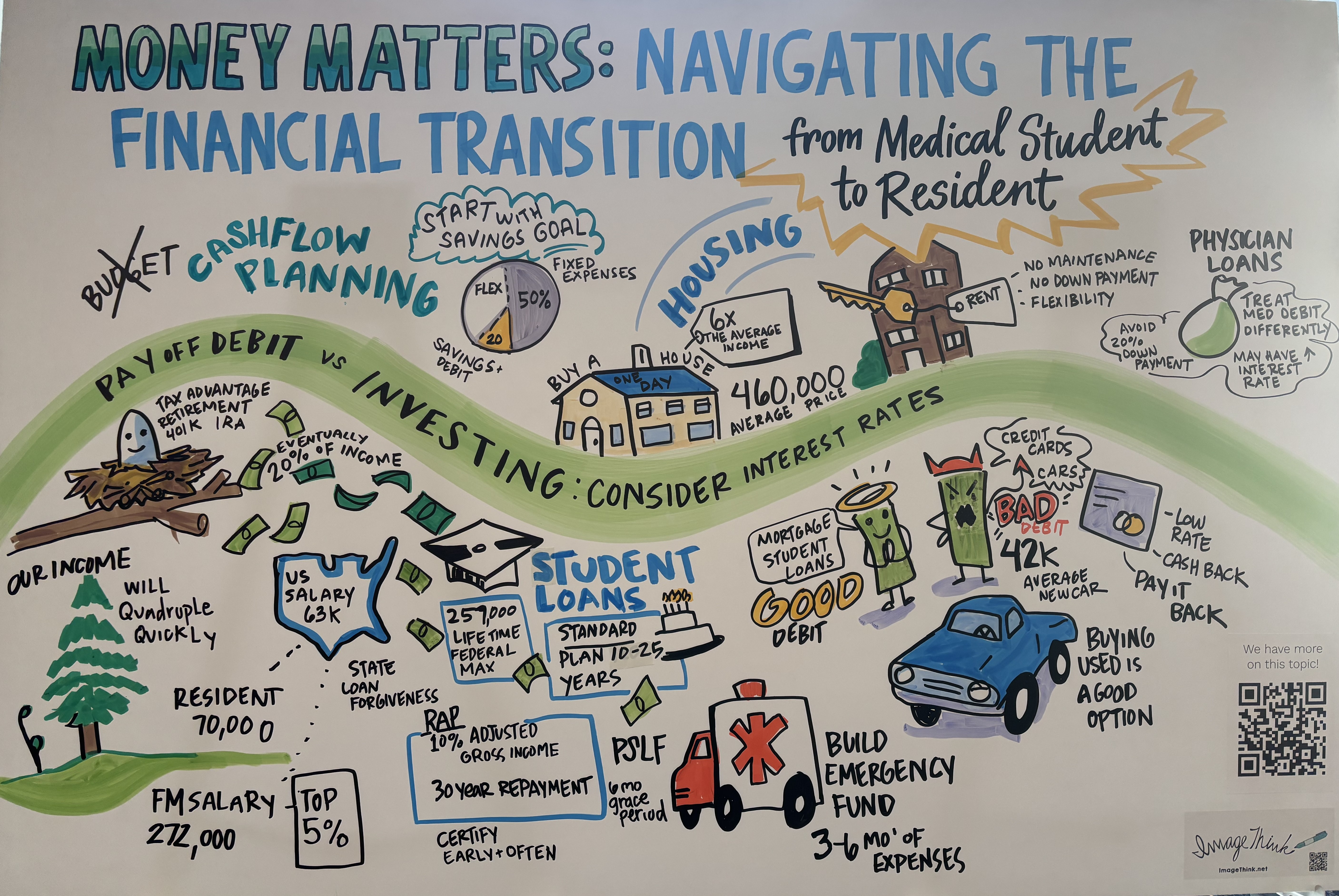
Related AAFP content: Managing Medical School Debt
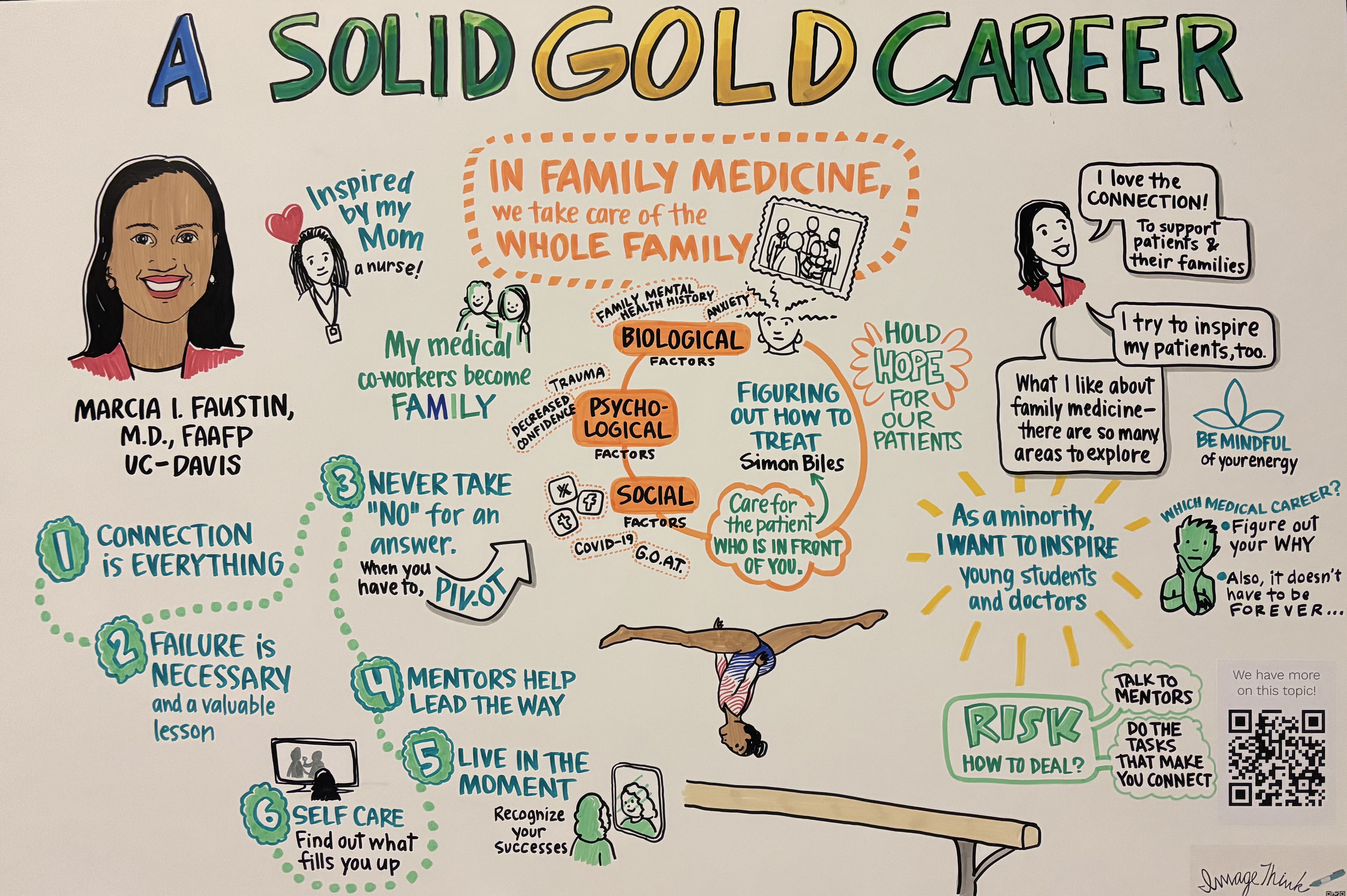
From Chicago to the Olympics: A Family Medicine Journey
Dr. Marcia Faustin's main stage presentation at FUTURE conference exemplifies how family medicine can serve as the foundation for extraordinary patient care, even at the highest levels of athletic competition. As the team physician for USA Gymnastics who cared for Simone Biles during the Tokyo 2020 Olympics, Dr. Faustin demonstrates that family medicine's emphasis on whole-person care easily translates from clinic rooms to Olympic arenas.
Her presentation showcased family medicine's versatility and the specialty's unique ability to provide comprehensive, relationship-centered care in any setting. Dr. Faustin's journey from a track athlete at Loyola University to an Olympic team physician illustrates that family medicine opens doors to unexpected opportunities while maintaining its core mission of caring for entire families and communities.
Five Takeaways for Medical Students and Residents:
- Connection is Everything: Foster deep relationships with family, friends, mentors, and patients—they serve as your foundation for success and life raft during challenging times.
- Embrace Failure as Growth: Setbacks, like Dr. Faustin's initial MCAT failure, often redirect you toward better opportunities and teach resilience that’s essential when you’re practicing medicine.
- Never Accept "No" as Final: When pursuing your goals, don't waste your energy convincing skeptics that it could be different—pivot that energy toward finding alternative paths to success.
- Live in the Present: Make sure you appreciate what you’ve achieved rather than constantly striving for the next milestone. This can prevent burnout and enhances patient care quality.
- Use the Biopsychosocial Model: Whether treating Olympic athletes or your clinic patients, it’s important to address it holistically—evaluating biological, psychological and social factors—for the best patient outcomes.
“The best part of my job is to be a part of each person's journey. I think it's a blessing. I think it is a privilege for us to hear these stories and for our patients to tell us things they don't even tell their mother or their significant others. And you are the only person that gets to hear it. And that is an honor for us to have and to be able to connect and support people. To ensure they live a life that has meaning for them. That's what I love.” – Dr. Marcia Faustin
My Mission in Medicine: Craft Your Story
Why This Topic Matters to Family Medicine
Storytelling is a foundational skill for family medicine physicians, enabling authentic connections with patients, colleagues and communities. This presentation explored how personal narratives can create psychological safety, communicate values and foster meaningful relationships that are essential to comprehensive primary care.
Family medicine's strength lies in building long-term therapeutic relationships, and as one presenter noted, "We're very good at telling other people's stories, but not as good at telling our own, especially in medicine." Personal storytelling allows physicians to move beyond clinical credentials to share their authentic selves, creating deeper connections that enhance patient care and professional satisfaction.
The session introduced the Challenge-Choice-Outcome framework, demonstrating how structured narratives reveal core values. As emphasized, "Stories not only do we connect with our values by telling our story, but others connect to those values with us." This approach transforms routine introductions from resume recitations into meaningful exchanges that build trust and understanding.
Five Key Takeaways for Medical Students and Residents
- Use the Challenge-Choice-Outcome framework to structure compelling personal narratives that reveal your values. Challenge – why did you feel it was a challenge? Why was it your challenge? Choice – why did you make the choice you did? Where di you get the courage or not? Outcome – how did the outcome feel? What did it teach you?
- Choose "scars versus open wounds" - share stories you've healed from rather than current vulnerabilities.
- Create psychological safety through sharing group commitments and authentic vulnerability.
- Move beyond traditional CV explanations to share the real person behind the accomplishments. Sometimes we focus our conversations on our degrees.
- Apply storytelling practically in residency interviews, patient interactions and personal statements.
Storytelling empowers family physicians to ground themselves in their purpose while creating the meaningful connections that define excellent primary care.
Advocacy 101: Understanding AAFP's Legislative Work
Why This Matters to Family Medicine
Healthcare policy directly impacts every aspect of family medicine practice - from Medicare reimbursement rates that determine practice sustainability to student loan policies affecting the next generation of physicians. The AAFP is the profession's voice in Washington, DC, advocating on issues that shape the future of primary care. Understanding this advocacy work is crucial for medical students entering a field where policy decisions affect patient access, physician compensation, scope of practice and the healthcare delivery system itself.
The AAFP's 365-day advocacy approach focuses on four core areas: recognizing primary care's value, reducing administrative burdens, strengthening the family medicine workforce and improving healthcare delivery policies. Recent legislative wins include preserving Public Service Loan Forgiveness program eligibility and securing Medicare physician payment adjustments, while ongoing challenges include Medicaid reforms and workforce development funding.
Five Key Takeaways for Medical Students and Residents
- Your Voice Matters: Individual physicians can have significant impact through advocacy summits, speak-out campaigns, and direct constituent contact with representatives. Your personal patient stories are powerful tools for policy change.
- A Bipartisan Approach Works: The AAFP maintains influence by focusing on patient care rather than partisan politics, ensuring access to both Democratic and Republican lawmakers.
- Multiple Advocacy Pathways Exist: From completing a Speak Out to the AAFP ambassador programs, there are engagement opportunities matching every schedule and commitment level.
- Student Loan Policies Directly Affect You: Recent legislation capped graduate loans at $200,000 and eliminated Grad PLUS programs, making advocacy for educational funding personally relevant.
- Early Engagement Builds Career-Long Skills: Learning advocacy principles as students prepares you for ongoing policy engagement throughout your medical career, protecting both your practice and your patients' access to care.
“One of the questions we often get asked is, how do you define success in today's challenging environment? Historically, the thinking has been getting a bill passed by Congress and signed into law by the president is an example of success.
I would argue it's a bit more. It’s shaping the regulation that comes through the rule-making process. Many times the work we're doing is stopping bad things from becoming reality or attempting to. It’s moving people from a position of opposition to a position of neutrality through a lot of the direct conversations with lawmakers on Capitol Hill.” – David Tulley
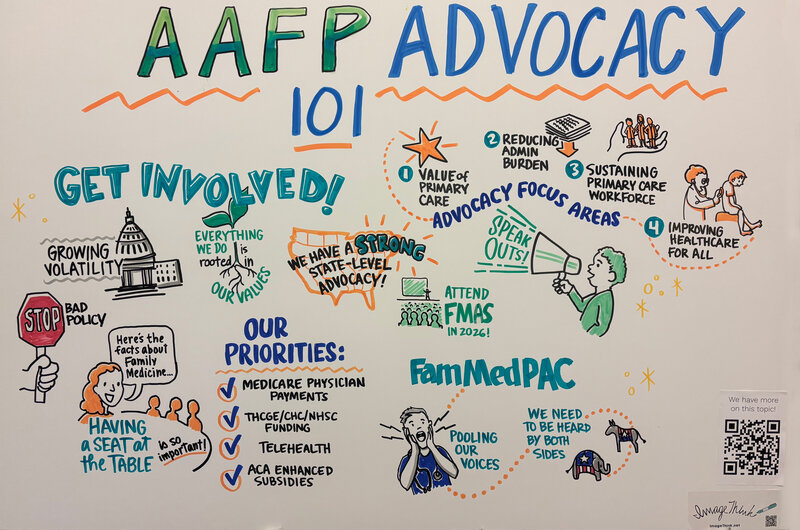
Related AAFP content: Advocacy: Fighting for Family Medicine
Direct Primary Care: Transforming Family Medicine Practice
Why This Topic Matters to Family Medicine
Direct Primary Care (DPC) represents an approach to addressing the systemic issues that plague American healthcare. With 63% of US physicians reporting significant burnout, 16 hours weekly spent on administrative tasks, and only 7 minutes of actual patient contact time during 15-minute visits, the current system is failing both doctors and patients.
DPC offers family medicine physicians a path to practice medicine as they were trained—with meaningful patient relationships, comprehensive care, and professional satisfaction.
Five Key Takeaways for Medical Students for Residents
- A Panel Size Revolution: DPC physicians manage ~600 patients versus 2,000-3,000 in traditional practice, enabling 30–60-minute appointments and same-day access.
- It Offers Financial Transparency: Monthly membership fees ($70-100 for adults, $20-50 for children) eliminate insurance billing, copays, and surprise medical bills while providing predictable healthcare costs.
- Improved Health Outcomes: Studies show a 40% reduction in ER visits, 53% reduced ER spending, 20% fewer hospital admissions, and better chronic disease management (39% improved A1C in diabetics).
- Physician Satisfaction is High: 94% of DPC physicians report job satisfaction versus 57% in traditional practices, with only 49% reporting burnout compared to 86% elsewhere.
- Practice Flexibility: DPC enables physicians to customize their practice, incorporate lifestyle medicine, perform more procedures, and maintain work-life balance while providing personalized care.
"Because I was able to take the time to listen to her... we did her entire work up to figure out she had been misdiagnosed 10 years ago. It's amazing what you can do when you actually have a chance to talk to your patients." – Dr. Tiffany Leonard
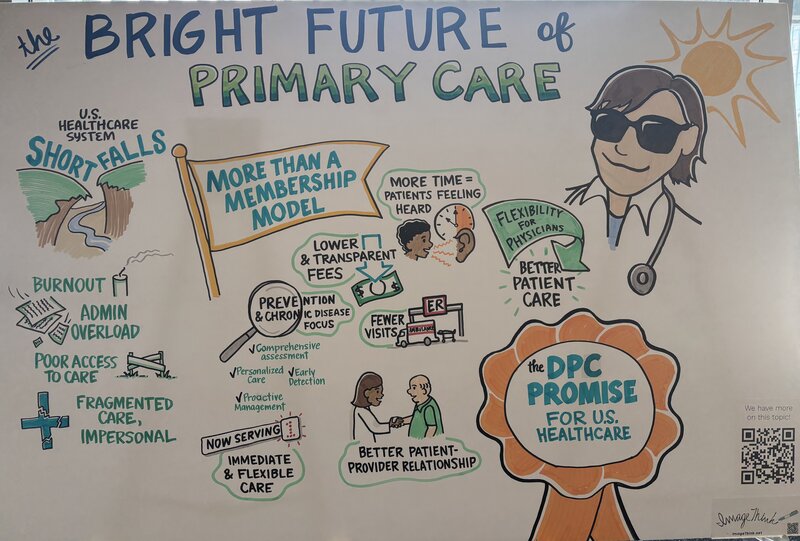
Related AAFP content: Direct Primary Care
Contract Negotiation in Family Medicine: A Critical Skill for Your Career
With 72% of family physicians now employed by health systems rather than private practice, mastering contract terms can significantly impact your career satisfaction, financial security and practice autonomy. This presentation equips medical students with practical knowledge to navigate their first employment agreement with confidence and avoid common issues that could affect their entire career.
Five Key Takeaways for Medical Students and Residents
1. Know Your Leverage and Market Value: Research compensation benchmarks using tools like the AAFP’s Career Benchmark Dashboard. Your strongest negotiating position is during your first contract - use it wisely. Rural and underserved areas typically offer higher compensation and signing bonuses due to physician shortages.
2. Understand Restrictive Covenants and Their Long-term Impact: Non-compete clauses can limit where you practice for 1-2 years after leaving. Many states now restrict these covenants for physicians. Ensure geographic limitations only apply to locations where you actually worked, not every system facility.
3. Negotiate Beyond Base Salary: Focus on signing bonuses, moving expenses, CME allowances and student loan assistance programs. These items often have more flexibility than base compensation due to anti-discrimination policies.
4. Secure Your Financial Protection: Ensure malpractice insurance includes "tail coverage" when you leave. Understand the difference between claims-made and occurrence policies, as tail coverage can cost 2x your annual premium.
5. Get Everything in Writing: Oral promises aren't enforceable. If it's not in your contract, you can't rely on it. Review all referenced policies and understand termination clauses, notice requirements, and outside employment restrictions before signing.
“Don't take the process personally. Just because they say no to your request doesn't mean they don't like you and they don't want you. They're constrained sometimes by their own heads or by legal principles of what they can do for you. So don't take it personally.” – Michael Burke, JD

Related AAFP content: Physician Employment Contracting
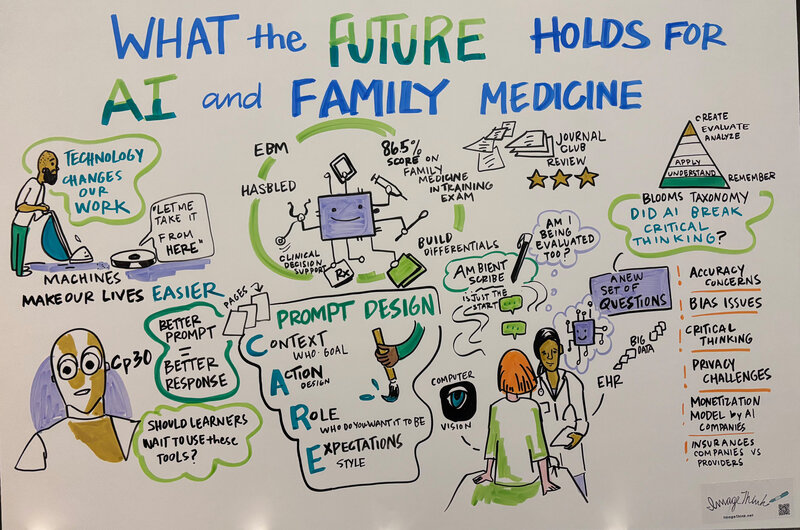
AI in Family Medicine: Transforming Primary Care Practice
Why This Matters for Family Medicine
As future family physicians, understanding AI's role is crucial for providing comprehensive, efficient patient care while maintaining the human-centered approach that defines our specialty. AI tools are already integrated into electronic health records, diagnostic imaging, and clinical decision support systems that you'll use daily in practice.
Family medicine's broad scope makes it uniquely positioned to benefit from AI's pattern recognition and decision support capabilities. However, the personal relationships and nuanced clinical reasoning that define family medicine require thoughtful integration of these technologies.
Five Key Takeaways for Medical Students and Residents
1. Master Prompt Engineering with CARE: Use the CARE framework when interacting with AI tools: Context (your background), Action (what you want it to do), Role (who you want the AI to be), and Expectations (desired output format). Quality prompts yield quality responses.
2. AI Enhances, but Doesn't Replace Clinical Reasoning: Large language models like ChatGPT can build differential diagnoses and explain complex concepts, but they complement—never substitute—your clinical judgment and patient interaction skills.
3. Embrace AI as a Learning Tool: AI provides personalized tutoring at your fingertips, adapting explanations to your learning level and offering immediate feedback on clinical scenarios.
4. Understand Current Applications: Ambient scribes, clinical decision support and evidence-based medicine tools are already transforming documentation and diagnostic processes in family medicine practices.
5. Navigate Ethical Considerations Thoughtfully: Consider disclosure, accuracy verification and maintaining critical thinking skills while leveraging AI's capabilities responsibly in patient care.
“As technology develops, our roles change. Of course, the question is – is primary care going to be taken over by AI? I hope you think absolutely not, at least not in our lifetime. Machines are helpful. Our computer systems are designed to assist us, not overtake our role completely. We are the creators of those machines, and ideally we're able to stay ahead of it.” – Dr. Karim Hanna
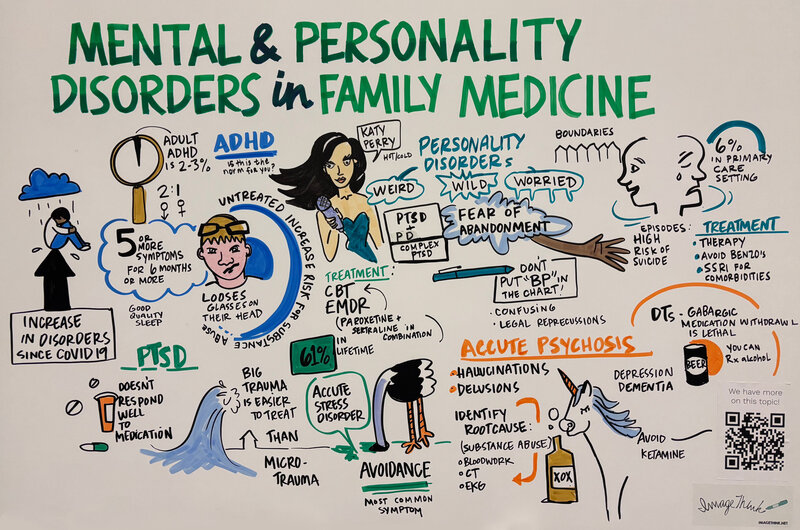
Mental Health in Primary Care: A Critical Component of Family Medicine
Mental health conditions represent a substantial portion of primary care visits, making psychiatric literacy essential for family physicians. This presentation addressed the wide variety of mental health issues encountered in family medicine clinics, providing practical diagnostic and treatment strategies for conditions ranging from ADHD to personality disorders.
Why This Matters to Family Medicine: Family physicians serve as the first point of contact for most mental health concerns. With limited access to psychiatric specialists, primary care providers must be equipped to identify, diagnose and manage common psychiatric conditions while recognizing when referral is necessary. The integration of mental and physical health care aligns with family medicine's holistic approach to patient care.
Five Key Takeaways for Medical Students and Residents
- Adult ADHD is Real: Don't dismiss ADHD concerns in adults over 18. Use the same diagnostic rigor as you would for children and remember that stimulants remain first-line treatment across all ages when clinically appropriate.
- PTSD Doesn't Respond Well to Medications: Trauma disorders require psychotherapy as the primary treatment. Avoid benzodiazepines in PTSD patients, as they can worsen outcomes and increase mortality risk.
- "Let Sleeping Psychotic Patients Lie": If an agitated patient is asleep when you enter the room, don't wake them up. This simple pearl can prevent unnecessary escalation.
- Borderline Personality Disorder is Possible: About 6% of primary care patients have personality disorders. Look for splitting behavior (you're either the best or worst doctor ever) and fear of abandonment as key diagnostic clues.
- Always Rule Out Medical Causes of Psychiatric Symptoms: Most acute psychosis cases are secondary to medical issues, substance use or withdrawal. Complete a thorough medical workup before assuming a primary psychiatric diagnosis that could follow them the rest of their life.
“A lot of what we think of when we think of trauma are these big events like the soldier who was in conflict or victims of a natural disaster like Hurricane Katrina. However, what the research has actually shown is that single large traumas are actually less difficult to treat than repeated long-term microtrauma. These patients with microtrauma have experienced people in their lives who say things like, oh, that's not a big deal, or why are you being so sensitive. But if you're from a family who repeatedly told you that you were overweight, then you're going to grow up with a lot of body image issues. There’s a lot of stress from that trauma.” – Dr. Boone Roundtree
Combating Medical Misinformation and Disinformation in Family Medicine
Why This Topic Matters to Family Medicine
Medical misinformation and disinformation represent critical challenges in family medicine, where physicians serve as primary communicators and trusted sources of health information for their communities.
As frontline providers, family physicians encounter conspiracy theories and false health claims daily, making it essential to develop effective strategies for addressing these issues while maintaining therapeutic relationships with patients.
Five Key Takeaways for Medical Students and Residents
- Distinguish Between Misinformation and Disinformation: Misinformation is wrong information, while disinformation is intentionally spreading false information with malicious intent to achieve personal gains.
- Use "Prebunking" Over Debunking: Research shows that warning patients in advance about potential misinformation they may encounter is more effective than trying to correct false beliefs after they've formed. This preventive approach aligns with family medicine's emphasis on prevention.
- Master the CRAAP Method for Evaluating Sources: When assessing information, consider Currency (is it current?), Relevance (does it answer the question?), Authority (who is the author?), Accuracy (how does it compare to other sources?), and Purpose (what's the motivation behind it?).
- Adapt Your Communication to Reading Levels: One-quarter of US adults read below a fifth-grade level, and the average reading level is eighth grade. Use plain language and avoid medical jargon to ensure effective communication.
- Empower Rather Than Dismiss: Building trust with your patients is essential. Acknowledge and even celebrate their analytical thinking, like the fact that they do a lot of research, while redirecting it toward reliable sources. Thank them for their concern and provide actionable steps they can take to protect their health.
"Conspiratorial thinking harms the trust that communities have in us. And it's that trust relationship between patient and doctor that is really the core of family medicine." – Dr. Sarah Coles
Related AAFP content: Countering Medical Misinformation Online and in the Clinic | AFP Editorial
Meet four family physicians who presented FUTURE workshops that reflect the broad scope of the conference. They share more about their passion areas and why the conference matters for future physicians.

Kalee Kirmer-Voss, MD, FAAFP
Presentation: Myths, Legends and the Truth About Family Medicine: A Workshop for the Inquisitive Mind

Sara Oberhelman-Eaton, MD
Procedure Carousel: A Rotation Through Multiple FM Procedures Using Hands-On Models & FMOB: A Hands-On Mini Boot Camp

Gretchen Irwin, MD, MBA
Presentation: Navigating Obstacles to a Successful FM Residency Application
David Schechter, MD
Presentation: Running a Private Practice Successfully
We’ve introduced you to some incredible student and resident leaders, and family physician presenters who love sharing knowledge with aspiring physicians. See what you missed.
Meet FUTURE event leaders
Kate Tran, MD: Resident leader hopes to help students find FUTURE in family medicine
Austen Ott: Student leader planning future in rural family medicine
Kamini Greer, MD: Program director brings passion for education to FUTURE
Mikala Cessac: I chose family medicine so I can care for the whole patient
Meet FUTURE presenters
Karim Hanna, MD: Speaker brings AI expertise to FUTURE
Benajmin Leong, MD: FUTURE speaker shows patients how food is medicine
Adam Shammami, MD: Award-winning mentor eager to ‘shape the next generation’
Learn what FUTURE offers
‘Invaluable’ leadership opportunities are open to students, residents
Past president: Students, residents play vital roles in AAFP leadership
‘Invaluable’ leadership opportunities are open to students, residents
