How to Use Modifier 25
Questions about modifier 25 have increased since add-on code G2211 was implemented in 2024 to reflect the value primary care physicians provide to patients. Learn how to report modifier 25 correctly so that you can get paid accurately.
What is modifier 25?
- Modifier 25 is a way to identify a “significant, separately identifiable evaluation and management service by the same physician or other qualified health care professional on the same day of the procedure or other service,” according to the CPT 2024 code set.
- Modifier 25 may only be appended to evaluation and management services.
When can it be used?
The E/M service must be significant and distinct from the procedure. The E/M must reflect work that is above and beyond the usual work associated with the procedure or other service.
Asking the following questions can help determine whether it is appropriate to use modifier 25:
✔️ Did you perform and document the key components of a problem-oriented E/M service for the complaint or problem?
✔️ As documented, could the E/M service stand alone as a billable service?
✔️ Is there a different diagnosis for this portion of the visit?
✔️ If the diagnosis will be the same, did you perform extra physician work that went above and beyond the work of the other service or the typical pre- or postoperative work associated with the procedure?
Modifier 25 should not be used when:
❌ The sole purpose of the encounter is for the procedure (e.g., lesion removal), and there is no documented medical necessity for a separate E/M service. The decision to perform a minor procedure is included in the payment for the procedure and should not be reported as a separate E/M service.
Example: Visit for lesion removal
A patient presents to have a mole assessed and the physician decides to remove it. The decision to remove the mole is included in the procedure code and should not be billed as a separate E/M service.
However, in this same scenario, if the mole has a suspicious, potentially malignant appearance that the physician relates to the patient, in a separate identifiable E/M service, and discusses the possible need for a more extensive procedure if the pathology report comes back positive for malignancy, the E/M visit would be reported with a 25 modifier, along with the procedure code for the lesion removal.
Rationale
- An E/M is related to and within the global period of a previously performed procedure. This includes minor surgical procedures (defined as a 000 or 010 day global period).
- Patient encounter is for a planned/scheduled minor procedure with no other, significant problems “addressed.”
- Patient encounter is for a preventive service, and there is no significant abnormality found that needs to be addressed within the components of a separate E/M office visit.

Understand how to properly document and code for E/M services.
What needs to be documented?
- Documentation must demonstrate the medical necessity of the E/M service.
- If possible, physically separate the documentation for the preventive service or procedure from the documentation for the problem-oriented E/M service within the patient’s medical record.
- Documentation should be able to support each service (i.e., the preventive service or procedure and the E/M) as though it were a standalone service.
Are separate diagnoses required?
No. An E/M service may be reported if it is clinically indicated and reflects work that is above and beyond the preoperative work associated with the procedure — even if both services have the same diagnosis. An example would be a patient who presents with a head laceration and you examine the patient for neurological damage before repairing the laceration.
Is modifier 25 required for E/M services provided at the same encounter as vaccines?
Yes and no. Traditional Medicare does not require modifier 25 for E/M services provided in conjunction with administration of the influenza (Healthcare Common Procedure Coding System [HCPCS] G0008), pneumococcal (HCPCS G0009) or hepatitis B (HCPCS G0010) vaccines. Medicare does require modifier 25 for E/M services provided in conjunction with other vaccine administration codes, including CPT codes 90480, 90460, 90461, 90471, 90472, 90473 and 90474. Private payers may have different policies. The E/M service must be significant and separately identifiable from the vaccine administration.
Can a preventive medicine visit and a problem-oriented visit be billed in the same encounter?
Yes. If a patient presents for a preventive visit and the physician identifies a new problem or changes to an existing problem that are significant enough to require additional work to perform the key components of the problem-oriented E/M service, both the preventive service and the appropriate office/outpatient E/M service may be reported. Append modifier 25 to the office/outpatient E/M service. While preventive and wellness services are not subject to cost-sharing, the office/outpatient E/M service may be subject to deductible and cost-sharing. If the problem is trivial and does not require additional work, an office/outpatient E/M service should not be reported.
For more information and examples, review the FPM article “Combining a Wellness Visit with a Problem-Oriented Visit: a Coding Guide.”
Do all payers follow the same rules for modifier 25?
Not necessarily. Traditional Medicare adheres to the National Correct Coding Initiative (NCCI). NCCI edits are updated quarterly. Some Medicare Administrative Contractors have NCCI Lookup tools available (Novitas, CGS Medicare, First Coast Service Options, Palmetto). Private payers often use their own claims editing systems and may not always align with Medicare. Review your payers’ policies or contact your local provider relations representative for more information.
How is the new add-on HCPCS code G2211 impacted by modifier 25?
Beginning January 1, 2025, Medicare will allow payment for G2211 when the base E/M services is appended with modifier 25 and provided on the same date as an annual wellness visit, initial preventive physical examination, vaccine or Medicare preventive service. A list of Medicare preventive services is available from CMS.
Where can I find more information about modifier 25?
You can find additional information, tools, and tips from the AAFP and the AMA.
- FPM Getting Paid blog: Seven quick tips for using modifier 25 (April 2023)
- FPM article: Combining a Wellness Visit With a Problem-Oriented Visit: a Coding Guide (January/February 2022)
- FPM article: Understanding when to use Modifier -25 (October 2004)
- FPM article: Getting Paid for Screening and Assessment Services (November/December 2017)
- AMA: Setting the record straight on proper use of modifier 25
- AMA CPT® Assistant: Reporting CPT Modifier 25
- CMS Medicare Claims Processing Manual, Chapter 12 and General Correct Coding Policies, Chapter 1.
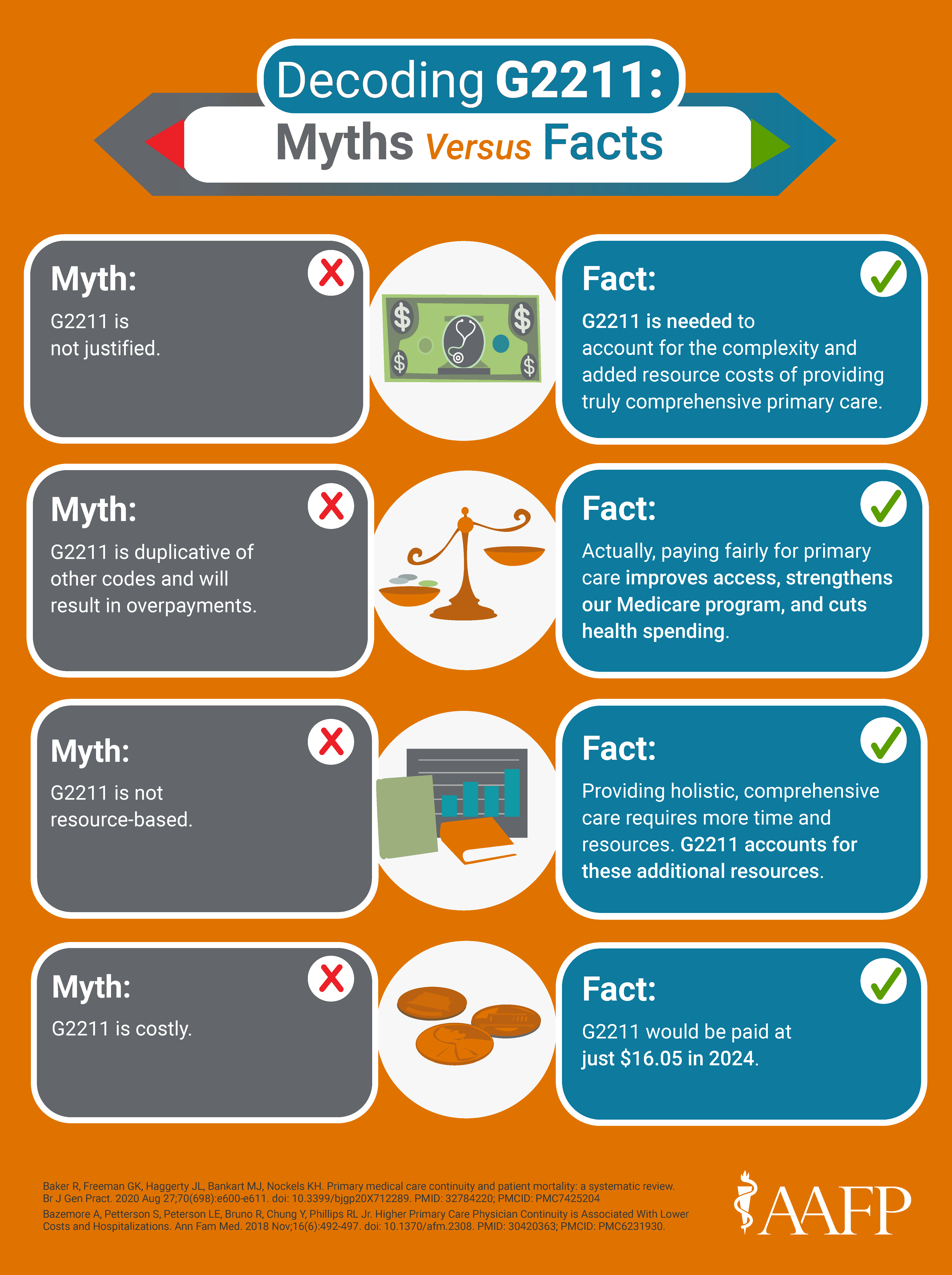
Use these G2211 tips to get paid accurately.