
If your relationship with an integrated organization seems tenuous, try to shore it up before you give up.
Fam Pract Manag. 2000;7(2):25-28
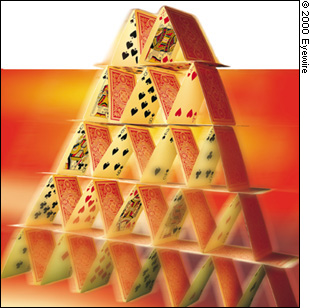
In the 1980s and early 1990s, health care integration was all the rage. You couldn't pick up a management journal without seeing advertisements for integration seminars. There was extensive talk about the benefits of merging into integrated systems under physician practice management companies (PPMCs), health care systems and hospitals. Not-for-profit hospitals were especially interested in building large, integrated entities under their leadership.
Now this trend has come under serious questioning. For a variety of reasons, hospitals, health care systems and PPMCs are learning that their investments in physician practices were ill-advised, and they're finding ways out. For the doctors, this can mean being given the opportunity to start up a new medical group, being forced to buy back their practices — or simply being unemployed. (For several examples of how family physicians are dealing with this situation, see “Disintegration: How Employed Doctors Are Landing on Their Feet,” FPM, November/December 1999, page .)
KEY POINTS:
Health care organizations are finding ways out of their investments in physician practices, leaving doctors to start new medical groups, buy back their practices or look for new employed positions.
As integrated organizations face rough times, doctors and their employers should try to focus on the benefits of integration that brought them together and rededicate themselves to accomplishing their original objectives.
For both the physicians and their employers, breaking up typically is much harder than staying together and working through the problems.
None of these possibilities is particularly welcome to the many physicians who saw in health care integration a way to escape the business of medicine. No sooner than many doctors had begun to get used to a new practice style that is characteristic of integrated organizations, the market entered into what some call the age of disintegration.
Still, many physicians aren't being fired or forced into practice buy-back; their marriages to larger health care entities are simply having rough times. Those doctors, and the entities that employ them, would do well to remember the benefits of integration that brought them together in the first place. For the doctors, those benefits typically include the larger organization's ability to negotiate better contracts with insurers, manage the delivery of services more effectively and market the practice (although realizing this potential requires focus and coordination by the organization). For both the physicians and their employers, breaking up typically is much harder than staying together and working through the problems.
So your first priority should be trying to accomplish your original objectives without dismantling the integrated organization. If, however, that proves to be impossible, approach your group's reorganization as if you were starting a medical group from scratch.
The trouble with integration
Responding to increased competition, hospitals and health care systems (beginning about a decade ago) saw the need to control networks so they could solidify referrals, especially in markets in which HMOs contracted on a discounted fee-for-service basis. The organizations, especially not-for-profit hospitals, began to buy physician practices, particularly those in primary care, so they could gain market advantage by building networks and improving service delivery.
Many of those organizations now operate their medical groups with ongoing losses. A survey of hospital-owned medical practices by the Medical Group Management Association and Medimetrix showed 75 percent losing money, with the losses averaging $60,000 per physician per year. A similar report by Ernst & Young also showed 75 percent losing money, with losses averaging $93,000 per full-time equivalent physician per year.1
According to Towers Perrin, hospitals expect to lose $43,432 per physician per year, even following best practices. This report also indicates that hospital-sponsored primary care networks lost an average of $83,290 in 1998, the range being $52,900 to $93,900.2 (See “Financial hemorrhaging at hospital-owned practices.”)
Overall, integration with a hospital seems no longer to be the strategy of choice. Many sources — and our experience — indicate that net income, patient volume, revenue from physician services, collections and total revenue for integrated physician practices are lower than they were before integration, and staffing is increased. Based on information like this, the surprise isn't that we're seeing disintegration but that the flood of divestitures doesn't yet appear to be a tidal wave.
Try to make it work anyway
Even in the face of data like this, integration remains a viable strategy in some situations. In some areas, physicians tend to have more realistic expectations about income, risk sharing and productivity demands since they have been working within organizations longer. In addition, some hospital CEOs are more realistic about their ability to control doctors, so they take more of a partnership approach. When these attitudes are present and the organization is prepared to engage competent management, integration can be a good strategy. But the integrated relationship must have these attitudes as its cornerstone, and all parties to the venture must buy into them.
Another reason integration can be effective is that, to some degree at least, bigger is better. Organizations that are large, proactive and efficient have greater potential to minimize the negative impact of market competition.
In many cases, integration efforts fail because of problems with the specific situation, not the strategy itself. It's probably fair to say that many of the ventures fail because the parties are rigid, have inflated expectations and are ill-prepared to function together. Often, a deal simply fails to produce partnership. Thus, physicians who face an unhappy marriage should seek first to strengthen the relationship. To do so, ask yourself the following questions to identify where the problems may lie:
Were the physicians' expectations too ambitious?
Was the capitalization insufficient to bridge the transition gap?
Did all parties fully understand the deal?
Did the hospital fully understand the business it was getting into?
Are all parties trying to build the best, most effective organization they can, or are they jockeying for position and pursuing policies to advance their own interests?
Has an adequate level of physician involvement been maintained?
Has everything possible been done to ensure good management? Doctors too often end up as highly paid production workers despite their having management skills that could be tapped (through incentives) to improve the organization. In addition, equipment and facilities often aren't used optimally.
Did the parties gain adequate buy-in from their constituencies before integrating?
Once you've identified the problems with your integration arrangement, you can assess whether the organization can be rehabilitated. Just because the boat is taking on water doesn't mean you can't plug the holes and sail on, taking a vigorous new approach to identifying problems, resolving issues and thus realizing the original objectives. If the answers to the questions above make you think that your relationship may be salvageable, follow these steps:
Revisit the initial goals and expectations of all parties to the deal.
Develop a remedial plan complete with priorities and a schedule. That plan should include extensive re-engineering to strengthen the relationship — perhaps a new strategic plan, a different approach to physician compensation and staffing to make the practice more competitive, a plan to enhance growth, risk-sharing arrangements, and incentives for good management and performance as an organization.
Ensure that the physicians buy into the remedial plan, including its goals and expectations.
Ensure that the hospital buys into the need to rehabilitate the practices' management and governance.
Revise the compensation program based on the organization's needs, and include appropriate performance incentives for physicians.
The bottom line is that you should seek opportunities to restructure the relationship in ways that will produce opportunities for both parties. Disintegration may seem likely, but it's probably in your interest to avoid that outcome. It's costly, time-consuming, risky and can require capital for practice buy-backs. And remember that even if you strike out on your own again, you probably won't be able to recapture the “good old days.”
Financial hemorrhaging at hospital-owned practices
Physician practices have proven to be of dubious financial value to the entities that bought them. One survey of 105 organizations employing or serving as the contracting entity for primary care physicians found the following distribution of losses:
| Gain or loss (per physician) | Percentage of practices |
|---|---|
| Gain of any amount | 16% |
| Loss of less than $25,000 | 17% |
| Loss of $25,000 to $50,000 | 19% |
| Loss of $50,000 to $75,000 | 16% |
| Loss of $75,000 to $100,000 | 14% |
| Loss of more than $100,000 | 14% |
Disintegration options
If you can't heal the relationship and find that you need to take back your medical practice, you'll have to create some good new days instead. Physicians facing disintegration have several options, including these:
Operate the practice independently. This option may align best with the temperament of the physicians; it gets them back in the management game and it can produce success. On the other hand, capital for practice buy-back isn't easy to get because the investment community tends to view this option skeptically. In addition, doctors too often are looking for the good old days, which most markets will no longer support. Another stumbling block is that physicians seeking to operate their practices independently often find that consensus among the doctors is extremely difficult to obtain and maintain.
Join forces with another established medical group. This option has a number of advantages: It results in increased market strength, it lets the doctors take advantage of existing management and operating systems, it minimizes disruption and it is less expensive. On the other hand, the doctors may discover that the “right group” is hard to find; potential partners are likely to be risk-averse; the new physicians may be seen as “second-class citizens” and may find partnership status hard to come by; and staffing issues often are problematic.
Find a different hospital or other organization with which to integrate. With this option, the doctors may be able to replicate their pay and working conditions, avoid consolidating facilities and avoid the need to raise initial capital. But this tends to be risky, and there are relatively few takers for these deals anymore. The organizations that are interested may simply be sticking their collective heads in the sand, and in this type of arrangement, the doctors would still be subject to decision making by nonphysicians.
Link up with a PPMC. As the experiences of companies like FPA Medical Management and MedPartners might suggest, PPMCs interested in acquiring practices today are extremely hard to find. Many PPMCs have a sour attitude about any company's ability to manage physicians and keep shareholders happy. In addition, the terms that physicians would receive most likely would be very different from the deals of the past, although they might be acceptable in markets where managed care doesn't dominate.
Due diligence
To determine what option would be best for your practice, you will need to approach disintegration as you would any major, new undertaking: with an effective due-diligence process. This may seem strange, particularly if you're planning to take back a practice you once managed. But keep in mind that the work of restructuring an integrated entity, or of dismantling it and starting the practice over independently, is as new and challenging as the original integration effort. Remember that the practice changed during the course of being integrated and that the infrastructure that is in place may not serve the medical group's needs once it becomes independent or enters into a different kind of integrated relationship.
In next month's issue of FPM, we'll discuss the issues that an effective due-diligence process should cover and first steps toward getting a reformulated practice up and running.