
This 32-site medical group was facing financial ruin, until its employees (both physicians and staff members) came up with a radical plan.
Fam Pract Manag. 2000;7(4):21-25

Integration was, for many physicians, the greatest hope of the early and mid-1990s. It promised them increased contracting clout with payers, enhanced infrastructure, improved practice operations and new revenue streams. But with few exceptions, these integrated organizations have not achieved their intended results and are suffering significant financial losses. Neither the hospitals nor the physician groups have realized their business objectives, and operating losses for medical groups have ranged from $10,000 to more than $100,000 per physician. In short, closing the integration deals has proven far easier than making these organizations financially and operationally viable.
But while the scenario of an organization acquiring physician practices and failing to realize its business plan is not unique, our story is. Rather than give up on the deal, our employed group of primary care physicians decided to redesign itself to achieve financial stability.
KEY POINTS:
Facing operating losses of $15 million, this employed primary care group had to “right size” its 32 sites and 120 physicians and midlevel providers.
An evaluation matrix enabled the group to compare its sites across multiple variables, both financial and nonfinancial, objective and subjective.
The practices are now focused on becoming an efficient, clinically distinctive medical group.
The history of EMG
In 1995, two nonprofit hospitals aggressively acquired 38 private physician practices and a health care plan to attract new “lives” and expand market share in the Denver metro area. The physician practices were joined together into a new group called Exempla Medical Group (EMG), composed entirely of primary care physicians. From the outset, EMG failed to achieve the economic projections of its business plan because, as we've learned from hindsight, simply acquiring many small practices and calling them a group does not create a true group organized to achieve common objectives. Adding to the troubles, the system itself had secured few, if any, new contracts, its health plan had failed to grow significantly, EMG physicians were guaranteed salaries based on historical revenue with no effective production incentive, reimbursement from payers was flat or decreasing, and infrastructure costs were extraordinary.
In 1996, the original business plan was discarded, and by May 1998, in its third year of operation, EMG was operating 32 sites and had annual operating losses of $15 million. Fearing additional losses, the parent organization then challenged the physician group with an almost inconceivable task: to break even by the end of 2000. The governing body of the medical group accepted the challenge and appointed a task force of physicians and staff members to spearhead the effort to reduce operating losses and improve revenue. The task force was to accomplish this by redesigning the group's 32 practice sites and 120 physicians and midlevel providers — hardly a small task.
To make the process fair and manageable, the task force divided it into three distinct steps:
Create an evaluation matrix that would allow side-by-side comparison of practice sites across multiple variables.
Test the financial impact of various redesign scenarios suggested by the evaluation matrix.
Implement the final plan according to an agreed-upon timeline.
1. Create an evaluation matrix
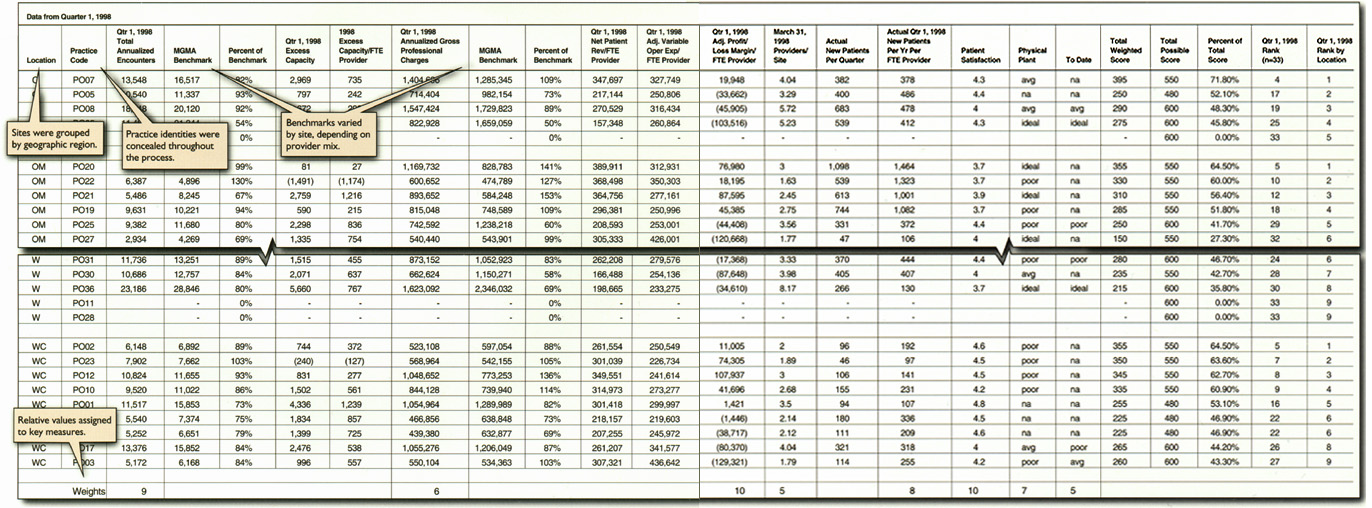
To determine which sites should be candidates for closure or consolidation, the task force needed some method for comparing all 32 existing sites. The tool we developed for this was an evaluation matrix that would calculate a total weighted score for each practice based on multiple criteria applied uniformly to all practices. (See the matrix below.) Knowing that the process could become emotional and political, the task force decided from the outset to blind all data and develop unique identifiers at both the physician and site level. The identities were shielded throughout the discussion and recommendation phases; however, sites were identified by geographic region so that the task force could maintain the group's presence in the Denver metro area as it explored redesign scenarios.
A critical step in the matrix development process was selecting the criteria the task force would use to evaluate each practice. It rejected the simple solution of closing sites based solely on profitability (net income or loss). Although this solution is both quick and an acceptable realms of business, it would not help us achieve our goal of creating a high-quality group of physicians that could be competitive and distinctive in our local market. Thus, the task force agreed that in addition to using traditional economic measures in the evaluation matrix (patient encounters, professional charges, operating expenses, etc.), it would also include important subjective factors, such as patient satisfaction and physician reputation. What resulted was a list of criteria that we believe define a successful practice. (See the full list below.)
Once the task force had identified the evaluation criteria, it then had to decide the relative importance of each criterion in defining a successful practice. Relative values (or weights) were assigned to each criterion that factored into the sites' final rankings (see the matrix for more explanation). The highest weights were given to patient satisfaction, profit and loss margin per FTE provider and annualized patient encounters, which we believe best determine a successful, high-quality EMG practice.
Measures of success
As part of its group redesign effort, Exempla Medical Group (EMG) used the following criteria to evaluate and compare the overall performance of its 32 practice sites. Together, these measures define a successful EMG practice.
Traditional measures
Annualized patient encounters (visits)*
Excess capacity
Annualized gross professional charges*
Net patient revenue per FTE provider
Adjusted variable operating expenses per FTE provider
Adjusted profit/loss margin per FTE provider
Providers per site
New patients per quarter
New patients per year per FTE provider
Subjective measures
Patient satisfaction (measured using a common tool over the previous 18 months)
Physical plant (ideal, poor or average)
Effectiveness of practice's marketing efforts within the last year to increase patient volume (ideal, poor or average)
Presence of a “magnet” provider
Value of a mix of specialty primary care providers
Potential for growth
Impact (current and potential) on managed care contracts
*Expressed as a percentage of benchmark data for the region and specialty obtained from the Medical Group Management Association.
2. Test the redesign scenarios
Once the evaluation matrix had identified the practices that were likely candidates for closure or consolidation, the task force tested a variety of group redesign scenarios to understand their impact on the group and to validate the final plan. For example, if sites 3 and 17 were consolidated, how would that impact group revenue? If site 8 were closed, what would that do to patient volume?
To analyze the potential volume and revenue changes resulting from the various redesign scenarios, the task force took into account two key variables:
One-time costs of redesign, which can be substantial, such as lease buy-outs and severance costs;
Potential savings that could be gained through the redesign, although perhaps not immediately, such as increased productivity, improved staffing ratios and reduced occupancy costs.
In our case the projected costs of redesign were approximately equal to the first year's savings, although ongoing savings were substantial. Ultimately, the model clearly identified which sites were the most logical candidates for consolidation or closure, and the task force recommended that the number of sites be reduced from 32 to 20.
With the evaluation of the sites finally complete, the group then had to face the more difficult decision: Which individuals should be members of the group? In deciding this, the leadership took into account seniority, primary care specialty, patient volume and individual physicians' interest in remaining in the group, and again we tested the various scenarios. In the end, 33 out of 120 physicians and midlevel providers left the group, with some resigning or retiring. In addition, we were forced to terminate only a few staff members and were able to transfer qualified staff into vacancies in other practices.
3. Implement the plan
With the final composition of EMG formally endorsed by the group's governing body and the parent organization's Board of Directors, it was now time to implement the redesign. One of our key concerns was alleviating hardship on individuals who would be leaving the group. We honored the physicians' employment contracts, which ranged from five-year guarantees for “founder” physicians to 90-day termination without cause for “associates.” We also wanted the process to happen quickly (within 90 days), rather than prolonging it. Within two days of the decisions, on-site meetings were held with each office and a physician leader notified all physicians in person.
Implementation turned out to be extremely labor intensive and involved a number of administrative and human resource tasks:
Defining the group's policies on leave and severance packages for both staff members and physicians,
Notifying payers of the changes within the group,
Helping patients affected by the terminations find alternatives that fit their personal needs and insurance requirements,
Terminating or buying out various leases held by the group.
A timeline of these and other tasks was developed for each office and each physician, which ultimately kept us on track and helped the implementation go smoothly.
An evaluation matrix
The evaluation matrix shown here in an abbreviated version enabled a side-by-side comparison of Exempla Medical Group's 32 practice sites. The “total weighted score” for each practice was based on eight key measures:
Total annualized encounters,
Annualized gross professional charges,
Adjusted profit/loss margin per FTE provider,
Providers per site,
New patients per year per FTE provider,
Patient satisfaction,
Physical plant,
Marketing.
Additional measures were considered in the comparison but not factored into the final score. Scores for the key measures were then converted into raw scores and multiplied by assigned weights to determine the total weighted score and final rankings.
To download a working copy of the full matrix, see the instructions. You will need Microsoft Excel to view the file.
Results
Thanks to the continued support of the physician governance group and the ongoing work of the management team, EMG's consolidation plan was nearly complete by the close of 1998. The results through 1999 are encouraging. With 33 fewer physicians and midlevel providers and 12 fewer sites, EMG has seen only a 1 percent reduction in total visits compared to 1998. Although net revenue has decreased 6 percent, total expenses have decreased 25 percent, making 1999 losses almost half of 1998 losses. Physician compensation is still above the target of 40 percent of net revenue, but nearly all of the sites are operating at or below budget. Lease costs for unoccupied space from the closed sites continue as a significant expense, as do severance packages, including guaranteed salaries for a portion of the group.
Nevertheless, for the Denver market in 2000, it appears that less is more. EMG now includes 87 physicians and midlevel providers who recognize that individual effort is an important part of group results. The group anticipates a break-even result by 2001, and given the results over the last year, we believe that goal is realistic.
Ultimately, downsizing, right sizing, redesign and consolidation are but tactics to stave off bankruptcy. With that problem nearly behind us, we can now focus on becoming an efficient, clinically distinctive medical group. Although there is likely no one model that will guarantee success, we are beginning to understand what we must do well in order to succeed:
Review and consistently assess what is succeeding within the group, what is failing and why;
Maintain a flexible operating philosophy to permit rapid adjustments in the group's course, partners, alliances and goals;
Define the group's values and create measurable goals based on those values;
Clearly state and constantly analyze economic expectations of each partner in the system; Maintain financial viability independent of a sponsoring organization;
Preserve high-quality medical care for our patients and community;
Ensure physician participation in the design and implementation of any new plans for the group.
This is indeed a new era in the delivery of health care. Although the models that will succeed remain undefined, it appears that physician groups, no matter how they are configured, now require unprecedented attention to business discipline. Those who hope to succeed must find a way to combine a well-run business with a commitment to improving patient care and community health.
Instructions for using the matrix
The practice evaluation matrix used by Exempla Medical Group is
. Although the group’s personal data has been altered in this version, the matrix itself is intact, allowing users to view the formulas and understand how the matrix works.
Notes:
Familiarity and competence with Microsoft Excel is necessary to use the matrix effectively.
The matrix was designed specifically for Exempla Medical Group and may not be easily transferable to other physician groups without some significant modifications.
Benchmark data used in the original evaluation matrix was taken from the Medical Group Management Association (MGMA) “Physician Compensation and Production Survey” from 1997 using 1996 data. More current data is available from the MGMA.
Functionally there are three components to the matrix:
1. Input.
Practices applying the matrix to their own situations would need to input into the following items:
Practice names and/or codes: Actual names of the physician practices, or codes that represent the physician practices, must be input to identify each line.
FTE (full-time equivalent) providers by specialty: These values are critical to calculating a weighted benchmark if the practice is a multispecialty primary care practice. The existing matrix has two sections for input, for use with different variables. This would not be necessary in all cases.
Data associated with the evaluation variables (e.g. encounters, revenue, expenses).
Weighting values: Based on the variables selected, weights are assigned to reflect the relative value or importance of each variable relative to the others. The weights we chose are shown in the sample matrix.
2. Raw score calculation.
Raw scores for each variable are calculated based on the actual value’s deviation from the benchmark or mean for that variable. To achieve a balanced distribution of raw scores (i.e., to prevent all practices from falling into one category), it may be necessary to adjust the amount of deviation from the benchmark that is necessary to trigger a higher or lower score. For example, a raw score of 5 may be assigned to values that fall within 25 percent of the mean or total values that fall within 50 percent of the mean, etc.
We used raw scores of 0, 5 and 10. These values were selected arbitrarily to achieve some level of differentiation in addition to the weighting. Any set of incremental values could be used.
3. Weighted score calculation.
Weighted scores are simply calculated by multiplying the raw score by the weighting value for each variable. The total score is the sum of all weighted scores.
For the original use of this matrix, it was necessary to calculate a total possible score and evaluate each practice with respect to how they scored relative to the total possible. This was due to the fact that many practices were not evaluated on some criteria, including marketing and physical plant.
Ranking was based on the percentage of the total possible score. Rankings were performed both overall and by geographic location. We also included rankings from the prior year to attempt to identify trends in performance relative to the other practices in the group.
Finally, it should be noted that any quantitative variables may be used in this matrix. In actuality, there were many iterations of this matrix, some having only four variables.