
Four key design elements could make your team more effective.
Fam Pract Manag. 2013;20(2):20-24
Author disclosure: no relevant financial affiliations disclosed.
Primary care physicians face an overwhelming volume of work. According to one estimate, managing patients' direct patient care, chronic care, and preventive care needs in the current system would require 21.7 hours per day1 – clearly an impossible task for an individual physician. Many are now recognizing that a robust team is critical to managing the health care needs of a patient population. New work flows and clarified responsibilities can improve communication and collaboration between primary care physicians, nurses, medical assistants (MAs), health coaches, dietitians, mental health providers, and other professionals, and this has been a major focus of patient-centered medical home projects.2
A significant challenge that has not been addressed in the literature, however, is the redesign of ambulatory care work spaces to better accommodate medical home concepts, specifically team-based care. This article shares the work done and lessons learned by the University of Washington (UW) Neighborhood Clinics, the community-based primary care arm of UW Medicine, a large health system in the Seattle area. The Neighborhood Clinics have been successfully implementing patient-centered medical home capabilities for about five years, most recently the team-care concept. The approval of a budget to build two new clinics and significantly remodel and expand a third created an opportunity to design clinics that specifically support team care as well as other elements of the patient-centered medical home. In designing the first of these new spaces, our Ravenna Clinic, we identified the following goals:
Develop work areas that promote coordination and communication between team members,
Design spaces that are patient-friendly, reducing patient anxiety by ensuring privacy, comfort, and a clear understanding of the care plan,
Design a flexible space that can accommodate day-to-day variations as well as long-term changes in primary care models,
Use space efficiently to reduce waste and cost,
Promote patient safety and decrease error through standardization in design and equipment and by placing needed equipment in exam rooms,
Integrate appropriate technology.
The clinic space that resulted from this work is attractive, functional, and efficient. It is an exemplar for other practices looking to design a new clinic or remodel an existing one to support the principles of the patient-centered medical home.
The problem with traditional clinic design
Ambulatory medical offices have typically been designed for small groups, sometimes utilizing homes or small office buildings, with a limited number of clerical and clinical staff. Any design changes made usually involve reconfiguring the examination rooms, while adjustments for front and back office work areas are usually minor. Little consideration is given to how patient-care teams might work together and how the office design might support or hinder their success.
Traditional office design impedes the effectiveness of clinical teams in the following ways:
Physicians and staff often work in different parts of the medical office. They rarely have a consistent line of sight to their fellow team members, which hinders communication.
Supplies and equipment required for patient care are often stored in special rooms remote to the patient room. This requires staff to leave the care area to acquire what they need, wasting time and steps.
Exam rooms within a given clinic often vary significantly in their layout, and supplies are stored in different locations within the exam rooms. Staff members waste time trying to orient themselves to each varied layout. With the addition of electronic health records (EHRs), computers and monitors are often shoehorned into exam rooms in ways that make interactions with patients (and computers) less effective.
Individual physician offices or consulting rooms isolate physicians from the team and reinforce hierarchy. The physician office also promotes “nesting,” particularly the accumulation of papers containing patient information, which then becomes inaccessible to the rest of the practice. Private offices also occupy expensive space that might be better used for direct clinical care.
Clinical staff work areas are often not located near exam rooms. Having designated work spaces for staff members promotes nesting.
Patient flow paths are often illogical and can confuse patients. Patients move through work areas where protected health information is stored and conversations regarding patient care are occurring. A clear space for “check out” at the completion of a visit is often missing, resulting in patients leaving the office without follow-up appointments, referrals, and post-visit instructions.
Four key design elements
Our clinic design efforts began with the creation of a work group to identify best clinical practices and incorporate them into the space design. This team included organizational and physician leaders, the physician service champion, clinic managers, and a national clinical care expert. The team worked in partnership with an architectural design firm and early in the process made site visits to several local medical facilities. A new clinic developed by the local children's hospital provided the best example of what we were hoping to achieve in developing a space to support team care.3
Following the site visits and work group discussions, we identified four key design elements for supporting team care, which were ultimately included in the design of our Ravenna Clinic.
1. On-stage areas optimized for patient flow. The notion of having on-stage and off-stage areas was developed by Walt Disney World Resorts as a way of ensuring that guests are minimally exposed to the “hustle and bustle that go on behind the scenes.”4 Our on-stage areas (the waiting/reception area, front of house, and exam zone; see the figure below) were designed to logically guide patients through the visit while reducing anxiety and feelings of isolation. The waiting/reception area is spacious, comfortable, and designed to shield patients from any behind-the-scenes work. Although front-desk staff are located in a separate work area away from clinical staff, they are kept updated on anticipated waiting times so they can inform patients of any delays. When an exam room is ready, an MA walks to the patient and greets him or her face-to-face, as opposed to simply calling for the patient across the waiting room. The idea is to treat each patient as a guest.
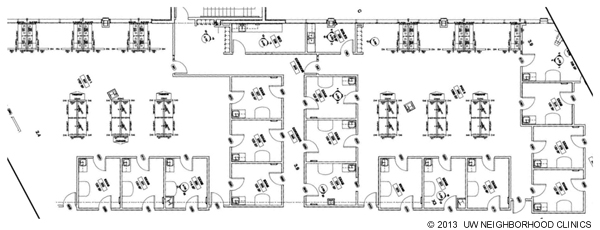
ON-STAGE AND OFF-STAGE AREAS
The UW Neighborhood Ravenna Clinic is divided into on-stage areas (the waiting/reception area, front of house, and exam zones) and off-stage areas (two team zones). The office layout is designed to move patients through the on-stage areas with ease and shield them from the hustle and bustle of the off-stage areas, where protected health information is stored and discussed among team members.

There is a single point of entry to the exam zone so that patients will not get confused. Color and carpet textures help designate patient areas and assist with way-finding. Windows not only provide light and create a welcoming environment but help orient patients so they can see where they are within the building in relation to, say, the parking lot or the front entrance. Doors separate hallways leading to off-stage team areas, while on-stage patient hallways remain open. Each exam room has two doors: one opening to the on-stage patient hallway and one opening to the off-stage team zone.
After the exam, the patient is escorted to his or her next destination. On-site lab and radiology services are positioned between the lobby and the exam rooms within the on-stage area. A check-out desk is located at the only patient exit. This allows us to engage with every patient exiting and ensure that all of their needs from the visit were addressed, including answering their questions and arranging follow-up visits, lab or imaging services, or referrals.
2. Standardized exam rooms. Exam rooms are standardized in their design and contain the same supplies and equipment stored in the same way. Vital signs, including weight and height, are measured in exam rooms, allowing for better patient privacy, greater convenience (patients have to unload their belongings, take off their shoes, etc., only once), and improved efficiency by reducing patient movement through the clinic. To facilitate use of the EHR, each exam room has a standardized workstation with a PC, a built-in printer, and a label printer. These tools also reduce wasted movement to obtain printouts and ensure that all specimens collected are immediately labeled by staff. The location of the computer monitor on a rounded desk next to the exam table allows the physician to access the medical record while still looking at the patient and allows the patient to see the monitor. Patients, MAs, and physicians can expect the same experience from room to room, cutting down on confusion for the patient and inefficiency for the physicians and staff.
Supplies are managed using lean principles. Cabinetry is kept to a minimum – only one cabinet per room – and there are no drawers, thus reducing the number of places to search for needed supplies. Instead of stocking every room for every possible procedure, we stock each room daily with a minimum amount of supplies in standard trays. Specialized carts and trays are available for situations requiring additional equipment or supplies, such as primary care dermatologic, orthopedic, gynecologic, and eye care procedures. These carts and trays are moved from the off-stage areas to the exam room when necessary. This approach significantly reduced the amount of space, equipment, and supplies needed in the exam room, in turn reducing the total amount of supplies in the clinic and minimizing the time spent discarding or recycling outdated materials.
3. Off-stage areas that put team members near one another. Off-stage areas are where most of the work of care teams is done. The key goal is to co-locate members of the care team to assist with easy communication and collaboration (see the figure below). For example, if a physician is located near his or her clinical staff members, an MA who sees a patient with a special need can easily inform the physician, thus improving the patient's experience and facilitating care. The nurse triaging a complicated patient on the phone can receive timely help from the physician, improving patient safety. A busy MA who is getting behind can ask another MA for help, improving office efficiency. All of this activity occurs in the “off-stage” area, never observable to or overheard by patients.
EXAM ROOMS AND TEAM AREAS
Exam rooms are bordered by the patient hallway, with the team zone in the center. All exam rooms have the same layout and contain the same supplies and equipment, reducing confusion and inefficiency. The clinic's off-stage area contains two team zones. Each is surrounded by the exam rooms the team uses. Both physicians and clinical support staff share these work spaces, as private offices do not exist. Locating all members of the clinical team together improves communication and collaboration.
Workstations are clustered together but have varying heights to avoid a sense of crowding and to allow for differing work styles (see the figure below). Exam rooms surround the work area, allowing a direct line of sight to patient rooms and other visual cues for all team members. The team can easily visualize which rooms are being used, who is in each room, and which rooms are available for the next patients. By using modular furniture instead of built-in cabinetry in these areas, we have retained the opportunity to adjust the layout for better efficiency as needed in the future.
Many design elements function to keep the team in the team area. Procedure carts and trays are located near the exam rooms, along with larger racks containing clinic supplies that are not in immediate use. Multiuse printers allow for scanning and faxing. High-definition radiology viewing stations are also located in the off-stage area. Resources such as vaccines and the soiled utility room are conveniently located in a centralized off-stage area.
A final element of the off-stage area concept is ensuring that space is available for team huddles to carry out daily planning. This procedure allows physicians and clinical staff to meet to review daily schedules, discuss any issues affecting patient care, review reports tracking key measures, and solicit feedback from one another.
While there was initial concern that these off-stage team areas would be noisy, experience has shown that co-location encourages quieter conversation. Although busy, the team area does not feel or sound chaotic.
TEAM WORKSTATIONS
Workstations in the team zones are clustered together but have varying heights to avoid a sense of crowding and to allow for differing work styles. Using modular furniture instead of built-in cabinetry in these areas allows for future adjustments to the layout. More secluded cubicles are available as well for phone calls, dictation, etc.

4. Shared space in lieu of private office space. The physicians in our workgroup agreed that physician offices separated from team work spaces were not efficient. However, the workgroup acknowledged that physicians need a quiet area to do their administrative work when they are not providing direct patient care. Shared cubicles at the back of the team zones were used to meet this need. The cubicles offer physicians and staff attractive, quiet spaces in which they can finish charting, dictate, complete paperwork, and make phone calls. Although loss of the physician office was met with significant resistance at the time of planning, physicians now tend to stay in the team area when involved in patient care, and the cubicles are infrequently used. The efficiency of being able to find staff to help them and the camaraderie of working in proximity to their colleagues outweighs the loss of private office space. Those few physicians who need a quieter space do move to the cubicles when they finish with patient care. Once we had our first clinic up and running with this new design, we were able to bring physicians and staff from clinics who were moving to this model into the new space during work hours to see how it functioned, which helped allay many concerns.
Not having private offices has also allowed us to incorporate larger open spaces into the design, including waiting rooms and conference rooms that were designed to accommodate group visits, provide meeting space, and provide teaching areas for medical students and residents as needed.
Lessons learned
To achieve the ambitious aims of the patient-centered medical home, practices may need a new architectural design. Our experience has shown us that care teams can be more successful if their work space is designed to support direct communication and collaboration, eliminate sources of waste and inefficiency, and ease the patient's journey through the clinic.
Significant changes in work flow and work space often meet with significant resistance. Early team communication about the goals of these changes, site visits to clinics with innovative designs, and involvement of the team in decision-making will help facilitate a successful outcome. Flexibility in design and implementation is also key, as each new project has individual needs and goals, and innovation in care delivery is an evolving process.
