
Am Fam Physician. 2009;80(4):356-362
Patient information: See related handout on hair loss, written by the authors of this article.
Author disclosure: Nothing to disclose.
Physicians should be careful not to underestimate the emotional impact of hair loss for some patients. Patients may present with focal patches of hair loss or more diffuse hair loss, which may include predominant hair thinning or increased hair shedding. Focal hair loss can be further broken down into scarring and nonscarring. Scarring alopecia is best evaluated by a dermatologist. The cause of focal hair loss may be diagnosed by the appearance of the patch and examination for fungal agents. A scalp biopsy may be necessary if the cause of hair loss is unclear. Alopecia areata presents with smooth hairless patches, which have a high spontaneous rate of resolution. Tinea capitis causes patches of alopecia that may be erythematous and scaly. Male and female pattern hair losses have recognizable patterns and can be treated with topical minoxidil, and also with finasteride in men. Sudden loss of hair is usually telogen effluvium, but can also be diffuse alopecia areata. In telogen effluvium, once the precipitating cause is removed, the hair will regrow.
Hair loss is a common problem that affects up to 50 percent of men and women throughout their lives.1 It can occur anywhere on the body, but more commonly affects just the scalp when the patient presents with concerns about the cosmetic effect. Family physicians need to be able to distinguish hair loss that represents true disease from the more common age-related hair loss. Hair loss is commonly categorized into scarring and nonscarring alopecia. Scarring alopecia is rare, and most cases of hair loss seen in primary care will be nonscarring. Hair loss on the scalp can be further classified as focal or diffuse. This distinction is the first step in diagnosis.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| In alopecia areata, there is no long-term benefit of topical steroids, minoxidil (Rogaine), cyclosporine, oral steroids, or photodynamic therapy. | A | 5 |
| Women presenting with hair loss associated with abnormal menses, history of infertility, hirsutism, unresponsive cystic acne, virilization, or galactorrhea should have a targeted endocrine work-up (i.e., testosterone, dehydroepiandrosterone sulfate, and prolactin). | C | 29 |
| Minoxidil 2% causes hair regrowth in female pattern hair loss. | B | 8 |
| Oral finasteride (Propecia) promotes hair regrowth in male pattern hair loss. | A | 12, 13 |
| Minoxidil 2% causes hair regrowth in male pattern hair loss. | A | 16, 40 |
| Discontinuation of finasteride or minoxidil results in loss of any positive effects of treatment (hair growth) in 12 and six months, respectively. | A | 13, 40 |
Differential Diagnosis
The causes of hair loss can be broadly divided into focal or diffuse hair loss (Table 1). Focal hair loss is secondary to an underlying disorder that may cause nonscarring or scarring alopecia. Nonscarring focal alopecia is usually caused by tinea capitis or alopecia areata, although patchy hair loss may also be caused by traction alopecia or trichotillomania. Scarring alopecia is rare and has a number of causes, usually discoid lupus erythematosus. Diffuse hair loss can be further categorized into conditions that cause hair shedding, of which the most common is telogen effluvium, and predominant hair thinning caused by male or female pattern hair loss (previously called androgenetic alopecia).
| Type of alopecia | Distinguishing characteristics | |
|---|---|---|
| Diffuse | ||
| Female pattern hair loss | Presents with hair thinning; frontal hairline intact; negative pull test away from hair loss | |
| Male pattern hair loss | Presents with hair thinning; M pattern; negative pull test away from hair loss | |
| Diffuse alopecia areata | Distribution more patchy; positive pull test | |
| Alopecia totalis or universalis | Total hair loss on the scalp and/or body | |
| Telogen effluvium | 30 to 50 percent of hair loss three months after precipitating event; positive pull test | |
| Anagen effluvium | Sudden hair loss of up to 90 percent two weeks following chemotherapy | |
| Focal | ||
| Nonscarring | ||
| Alopecia areata | Normal scalp with surrounding exclamation point hairs | |
| Tinea capitis | Scaly scalp with fungus visible on potassium hydroxide examination | |
| Traction alopecia | Patchy; related to hair practices; may have some scarring | |
| Trichotillomania | Patchy; may be some scarring and associated psychological disturbance | |
| Scarring (cicatricial) | Scarring and atrophy of scalp (e.g., discoid lupus erythematosus) | |
Focal Hair Loss
ALOPECIA AREATA
Alopecia areata is characterized by areas of nonscarring hair loss that range from single oval patches to multiple patches that can become confluent. Men and women are equally affected, and, although it can occur at any age, the most common presentation is in children and young adults, with 30 to 48 percent of patients affected before 20 years of age.2,3 Alopecia totalis is loss of all scalp hair, and alopecia universalis refers to loss of all scalp and body hair. In case series, alopecia totalis and universalis are less common than alopecia areata and account for 4.5 to 30 percent of all alopecia cases. The lifetime risk of developing alopecia areata is 1.7 percent, with a prevalence of 0.1 percent.2,3 There is a genetic predisposition to alopecia areata with a polygenic pattern of inheritance. In most studies, 20 to 42 percent of those affected have a family history of the disease.4 Skin biopsy from areas of alopecia may show multiple lymphocytes, which supports the theory for an autoimmune cause. Alopecia is associated with autoimmune conditions, such as vitiligo, diabetes, thyroid disease, rheumatoid arthritis, and discoid lupus erythematosus. Patients with a history of atopy are also at an increased risk of developing alopecia.
The patient with alopecia areata (Figure 1) typically presents with bald patches on the scalp that often have developed rapidly with sudden loss of hair. In diffuse alopecia, there is more widespread hair loss, often associated with graying of the hair. The classic finding is a smooth, hairless patch surrounded by so-called exclamation point hairs. These are 2- to 3-mm broken hairs that have a club-shaped root with a thinner proximal shaft and a normal caliber distal shaft on microscopic examination (Figure 2).
Treatment may induce hair growth, but usually does not change the course of the disease. When treatment is stopped, hair loss recurs. Many patients with one or two small patches can be managed without treatment and with reassurance of the benign nature of the condition. A systematic review of 17 randomized controlled trials of topical and oral steroids, topical minoxidil (Rogaine), topical cyclosporine, and photo-dynamic therapy found no long-term benefit of these interventions.5 In patients with persistent hair loss and less than 50 percent scalp involvement, intralesional corticosteroid therapy is the first-line treatment.6 Patients with more than 50 percent hair loss can be treated with topical immunotherapy using diphenyl-cyclopropenone or squaric acid (Table 25–18).7 Overall, 34 to 50 percent of patients with alopecia areata will recover within one year; this number is as high as 80 percent in patients with one or two patches.6 The more severe the disease at onset, the worse the prognosis, with fewer than 10 percent of patients recovering from alopecia totalis and alopecia universalis.19
| Treatment | Dosing | Strength of evidence | Comments |
|---|---|---|---|
| Alopecia areata | |||
| Topical steroids | Applied twice daily to scalp | B | Evidence for short-term growth, but none for long-term growth5 |
| Topical minoxidil (Rogaine) | Applied twice daily | B | Evidence for short-term growth; one study showed more hair regrowth with 5% than 1% formulation5,6 |
| Topical immunotherapy with diphenylcyclopropenone or squaric acid | Treatment applied by dermatologist every few weeks | B | Unlicensed treatment; may cause severe dermatitis7 |
| Oral steroids | Six-week tapering course of prednisone starting at 40 mg per day | B | Continued treatment is needed to maintain hair growth; risks of prolonged steroid use outweighs the benefits6 |
| Intralesional corticosteroids | Triamcinolone acetonide (Kenalog) 5 to 10 mg per mL; 0.1 mL injected with a 30-gauge needle into the dermis 1 cm apart to a maximum of 3 mL; can be repeated every four to six weeks | C | Hair regrowth lasts a few months; effect on long-term outcome is unknown6 |
| Anthralin cream (Dritho-Creme HP) | 0.5% to 1% cream once daily for 20 to 30 minutes, increasing by 10 to 15 minutes every two weeks | C | Hair staining prevents use in fair-haired patients6 |
| Female pattern hair loss | |||
| Minoxidil 2% | Apply twice daily to dry scalp | B | 20 percent of women using the drug versus 7 percent of women taking a placebo reported moderate new hair growth after 32 weeks; number needed to treat = 88; 7 percent of women using minoxidil experience undesirable hypertrichosis9 |
| Spironolactone (Aldactone) | 100 to 200 mg orally daily | C | 88 percent of women had a modest decrease in hair loss with treatment10 |
| Flutamide (formerly Eulexin) | 250 mg orally daily | C | Treatment for one year resulted in a modest improvement in alopecia; 32 percent of participants experienced elevated liver function tests while taking the medication, resulting in some safety concerns11 |
| Male pattern hair loss | |||
| Finasteride (Propecia) | 1 mg orally daily | A | Promotes hair growth for more than two years, with the effect waning by year three12,13; does not significantly affect sperm production and poses no risk to a female sex partner; when screening men on finasteride for prostate cancer, the upper limit of normal prostate specific antigen levels should be doubled to ensure appropriate interpretation14,15 |
| Minoxidil (2%) | 1 mL to scalp twice daily | A | Consistent evidence showing moderate to dense regrowth of hair16 |
| Minoxidil (5%) | 1 mL to scalp twice daily | A | Consistent evidence showing moderate to dense regrowth of hair16 |
| Ketoconazole (2%) shampoo (Nizoral) | Daily | C | Increased hair density, size, and proportion of anagen follicles after shampooing two to four times per week for 21 weeks17 |
| Pyrithione zinc (1%) shampoo (Head and Shoulders) | Daily | C | Increased total visible hair count, but 5 percent less than treatment with minoxidil 5%18 |
TINEA CAPITIS
Children are most likely to be affected by tinea capitis and typically present with a round patch of hair loss, often with scaling, erythema, and lymphadenopathy. In a study of the predictive signs and symptoms of tinea capitis in children, those with occipital adenopathy were more likely to have cultures positive for fungi (positive likelihood ratio of 7.6) than those children with only alopecia, pruritus, or scaling.20 If the diagnosis is not clear from the history and physical examination, a skin scraping taken from the active border of the inflamed patch can be put into potassium hydroxide and examined microscopically for the presence of hyphae. Skin scrapings can also be sent for fungal culture, but this is less helpful because the fungi can take up to six weeks to grow. Tinea is caused by the microsporum species, which fluoresces under a Wood lamp; however, in the United States, most tinea is caused by trichophyton, which does not fluoresce, so this test is less useful. In its most severe form, tinea capitis causes a boggy inflammatory mass called a kerion, which may heal with scarring and subsequent localized alopecia.
Tinea capitis can be treated with oral terbinafine (Lamisil), fluconazole (Diflucan), itraconazole (Sporanox), or griseofulvin (Grifulvin); topical treatments by themselves are not effective. Dosing of griseofulvin is 10 to 20 mg per kg per day for six to eight weeks in children21 or 500 mg per day for six to eight weeks in adults.22 Terbinafine is approved for treatment of tinea capitis in children and requires a two- to four-week course.23
TRACTION ALOPECIA
Traction alopecia is a form of unintentional hair loss associated with specific social, cultural, and cosmetic practices. Patients (primarily women) wearing wigs, tight braids, or using curling rollers are at risk. Hair processing including bleaching, coloring, and waving also puts patients at risk. Hair loss usually occurs in the frontotemporal area, although it can vary. Eliminating the stressor or source of traction on the hair commonly cures the problem and returns hair growth to normal. Several small case reports have shown topical minoxidil 2% to be beneficial for treatment.24 In rare circumstances, chronic traction can set in motion a process of folliculitis and subsequent scarring that can result in permanent hair loss to the affected area.
TRICHOTILLOMANIA
Trichotillomania is a psychiatric compulsive disorder that involves repeated hair plucking. It is most common in children, but may persist into adulthood. On close inspection, twisted and broken off hairs are visible in patchy areas across the scalp. In chronic cases, scarring alopecia may result.
CICATRICIAL ALOPECIA
Cicatricial or scarring alopecia causes permanent hair loss from destruction of the hair follicles by inflammatory or autoimmune diseases. The most common cause of this is discoid lupus erythematosus, which produces atrophied erythematous patches, sometimes with telangiectasia.
Generalized Hair Loss
TELOGEN EFFLUVIUM
Telogen effluvium occurs when an increased number of hairs enter the telogen (resting) phase of the hair cycle from the anagen (growing) phase, and these hairs are lost approximately three months later. Usually, an average of 100 hairs are lost each day, but this becomes significantly more in telogen effluvium, in which 30 to 50 percent of body hair can be lost. Telogen effluvium may be precipitated by severe illness, injury, infection, surgery, crash diets, psychological stress, giving birth, thyroid disorders, iron deficiency, anemia, or drugs. Hyperthyroidism and hypothyroidism can cause telogen effluvium, which is usually reversible when the thyroid status is corrected (except in long-standing hypothyroidism). Severe iron deficiency anemia may be associated with it, but this remains controversial.25,26 Drugs that cause telogen effluvium include antithyroid agents, hormones, anticonvulsants, anticoagulants, beta blockers, angiotensin-converting enzyme inhibitors, and lithium. No cause is found in approximately one third of cases.27
Patients with telogen effluvium usually present with an increased number of hairs in their hairbrush or shower, and sometimes thinning of the hair in the scalp, axillary, and pubic areas. A detailed history may indicate the cause of the hair loss, which usually has occurred two or three months before the hair falls out. On examination, there is generalized hair loss with a positive hair pull test, indicating active hair shedding, particularly at the vertex and scalp margin. The hair pull test is done by grasping approximately 40 to 60 hairs between the thumb and fore-finger and applying steady traction (slightly stretching the scalp) as you slide your fingers along the length of the hair. Generally, only a few hairs in the telogen phase can be plucked in this fashion. Less than 10 percent is considered normal, whereas greater than this is considered indicative of a pathologic process.28 Treatment of telogen effluvium primarily involves removal of the underlying stressors or correction of any precipitating medical conditions.
ANAGEN EFFLUVIUM
Anagen effluvium is the abrupt loss of 80 to 90 percent of body hair, which occurs when the anagen (growing) phase is interrupted. The main cause of this is chemotherapy.
FEMALE PATTERN HAIR LOSS
Up to 50 percent of women will experience female pattern hair loss during their lifetime.1 Patients usually present with hair thinning over the central area of the scalp and widening of the midline part, but with reservation of the frontal hairline (Figure 3). Women who also have abnormal menses, history of infertility, hirsutism, unresponsive cystic acne, virilization, or galactorrhea should have a targeted endocrine work-up for hyperandrogenism (i.e., testosterone, dehydroepiandrosterone sulfate, and prolactin), although most will have normal androgen levels.29 Evaluation for iron deficiency, thyroid disease, and syphilis (a rare cause) should be considered because they can contribute to hair thinning or generalized hair loss.

Minoxidil 2% is the only treatment approved by the U.S. Food and Drug Administration (FDA) for treating female pattern hair loss in women older than 18 years. A hyperandrogenic state may limit the success of treatment with minoxidil,30 and, in these women, spironolactone (Aldactone) 100 to 200 mg daily may slow the rate of hair loss.10,31 Women with evidence of a hyperandrogenic state requesting combined oral contraceptives would benefit from using antiandrogenic progesterones, such as drospirenone.32 Finasteride (Propecia) is ineffective in postmenopausal women with female pattern hair loss.33 Over-the-counter topical preparations, hair extensions, and hairpieces are available for women with poor response to treatment.
MALE PATTERN HAIR LOSS
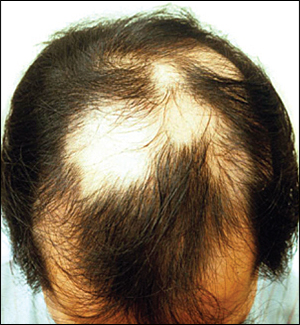
Male pattern hair loss (sometimes referred to as male androgenetic alopecia) affects up to 50 percent of all white men by 50 years of age.1 Although it is not life threatening, it is associated with negative psychological effects, including low self-esteem, depression, and a general dissatisfaction with body appearance.34 Hair loss affects the androgen-sensitive follicles, starting with bitemporal recession, and then spreads to thinning of the vertex and frontal regions in a classic M pattern. Dihydrotestosterone (DHT), the androgen derived from testosterone, plays a key role in male pattern hair loss, and men with lower levels of DHT have less hair loss.35,36
Topical minoxidil (2% and 5%) and oral finasteride are the only treatments approved by the FDA for treatment of male pattern hair loss in men older than 18 years. Treatment with finasteride can cause decreased libido, impotence, and ejaculation disorders.12 These adverse effects often abate with continued treatment and happen in less than 2 percent of men younger than 40 years.13 Finasteride may also induce depression.37 Minoxidil is available over-the-counter, and it should be applied to the scalp and not the hair. Its mechanism of action is unclear. Some shedding during the first few months of treatment is common. The minoxidil 5% solution has not been shown to be consistently more effective than the 2% solution, and patients using the higher concentration had more adverse effects, including allergic contact dermatitis, dryness, and itching.16 These typically resolve after treatment is discontinued.9
Several small studies have shown some increased effectiveness with combined minoxidil and finasteride treatment.38,39 Starting treatment early can help maximize success, and patients can expect to see results after three to six months, although dense regrowth is not likely. Discontinuation of finasteride or minoxidil results in loss of any positive effects on hair growth within 12 and six months, respectively.13,40 When switching between treatment with finasteride and minoxidil, it is best to overlap treatments for three months to minimize hair loss.41 Additional treatment options are listed in Table 2.5–18
Diagnostic Strategy
Begin by determining if hair loss is focal or diffuse; if focal, look for scarring. Patients with scarring should be referred to a dermatologist. In nonscarring focal alopecia, alopecia areata or tinea capitis are most common. In alopecia areata, the lesion is round and smooth, whereas in tinea capitis, the skin can look slightly scaly and erythematous, and there may be occipital adenopathy. A scraping of the lesion to evaluate for fungi may help. Traction alopecia and trichotillomania tend to cause more patchy hair loss and can usually be determined from the history. Consider a scalp biopsy if the diagnosis of the focal hair loss is not clear.
In diffuse hair loss, ask if the loss is predominantly hair thinning or shedding, if there is a relationship to any inciting event, and if there are symptoms of anemia, hyperandrogenism, or thyroid disease. The patient who presents with gradual hair thinning most likely has male or female pattern hair loss recognized by the typical patterns. The hair pull test will be positive where the hair is thinning, but negative away from the thinning areas. Patients with hair shedding may have telogen effluvium or diffuse alopecia areata, both of which cause a positive hair pull test. The history may reveal the precipitating event in telogen effluvium, whereas patients with alopecia areata may have exclamation point hairs. In all patients with diffuse hair loss, serum ferritin and thyroid function tests should be ordered.25,42 Syphilis is a rare cause of telogen effluvium, but should be ruled out if risk factors are present. Patients with suspected telogen effluvium can be observed until spontaneous resolution occurs, usually within six months, provided the provoking stimulus has been removed. If hair loss does not resolve, a scalp biopsy to differentiate between alopecia areata, telogen effluvium, and male or female pattern hair loss should be obtained.