Am Fam Physician. 2018;98(3):146
Author disclosure: No relevant financial affiliations.
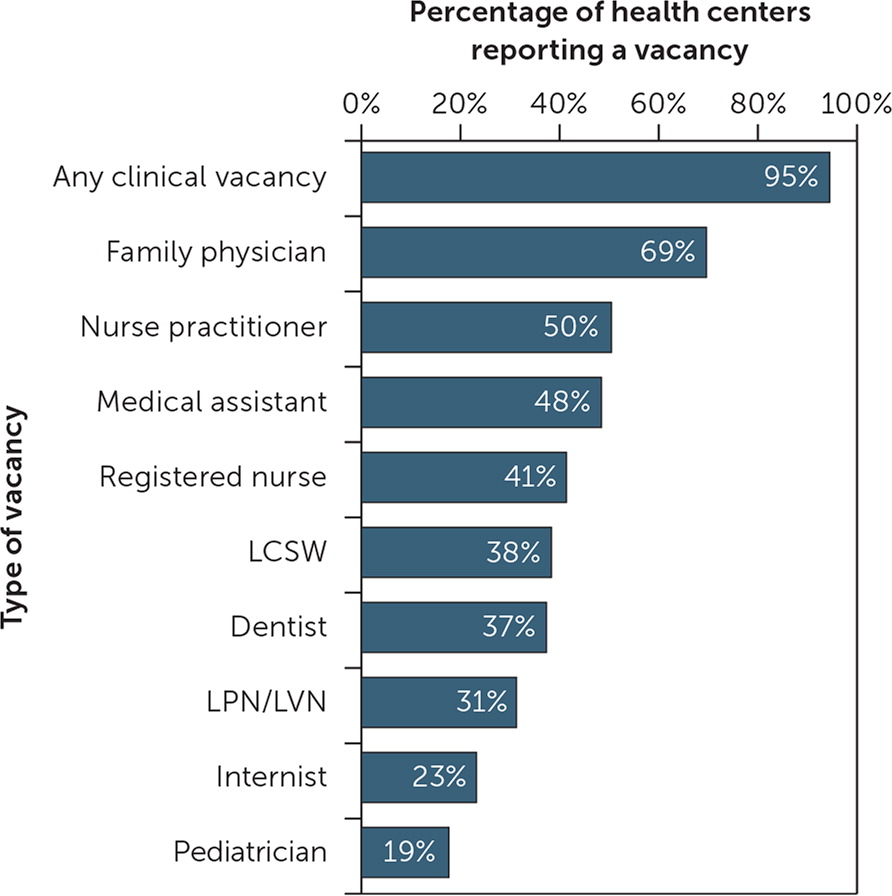
Expansion of the Health Centers Program has been associated with persistent workforce challenges for this critical component of the primary care safety net. In a national survey, 69% of health centers had a family physician (FP) vacancy. Those with FP vacancies reported spending an average of 11.4 months recruiting for an FP, one of the longest recruiting periods for a clinical position.
After years of bipartisan support for expansion, the Health Centers Program collectively delivers care to more than 27 million patients in more than 10,000 predominately low-income communities—substantial growth from the 10 million served in 2000.1 A 2006 health center survey revealed that 13.3% of FP positions were vacant, which was third highest among physician positions and fourth overall.2 More than a decade later, the National Association of Community Health Centers resurveyed health centers on their clinical workforce vacancies and their recruitment and retention experiences. Of the 1,278 health centers surveyed, 499 (39%) responded. Respondents were representative of health centers nationally based on characteristics such as size, patient insurance mix, and geography.3
Results of this assessment show that clinical vacancies are still common at health centers—95% report having at least one. Vacancies for FPs are the most common, with at least one at 69% of the health centers (Figure 1).3 In addition, 51% of health centers indicate that filling an FP vacancy is their highest priority. Two-thirds of centers rate FP vacancies as very difficult to fill, and those with FP vacancies spend an average of 11.4 months recruiting for FPs, one of the longest periods reported for any clinical vacancy.3
Although health centers employ a multidisciplinary health professional workforce to meet the diverse needs of their patients, nearly one-half (46%) of all health center physicians are FPs,4 and survey findings suggest that FP supply is not meeting demand. This highlights a need for policy makers to support federal programs that create incentives and provide community-based primary care training opportunities for medical students and residents to ensure an adequate supply of FPs to staff health centers and provide care to underserved populations.