
Am Fam Physician. 2022;105(6):602-612
Related Letter: Case Report: Delayed Diagnosis of a High-Grade Spindle Cell Sarcoma Presenting as a Thigh Mass
Author disclosure: No relevant financial relationships.
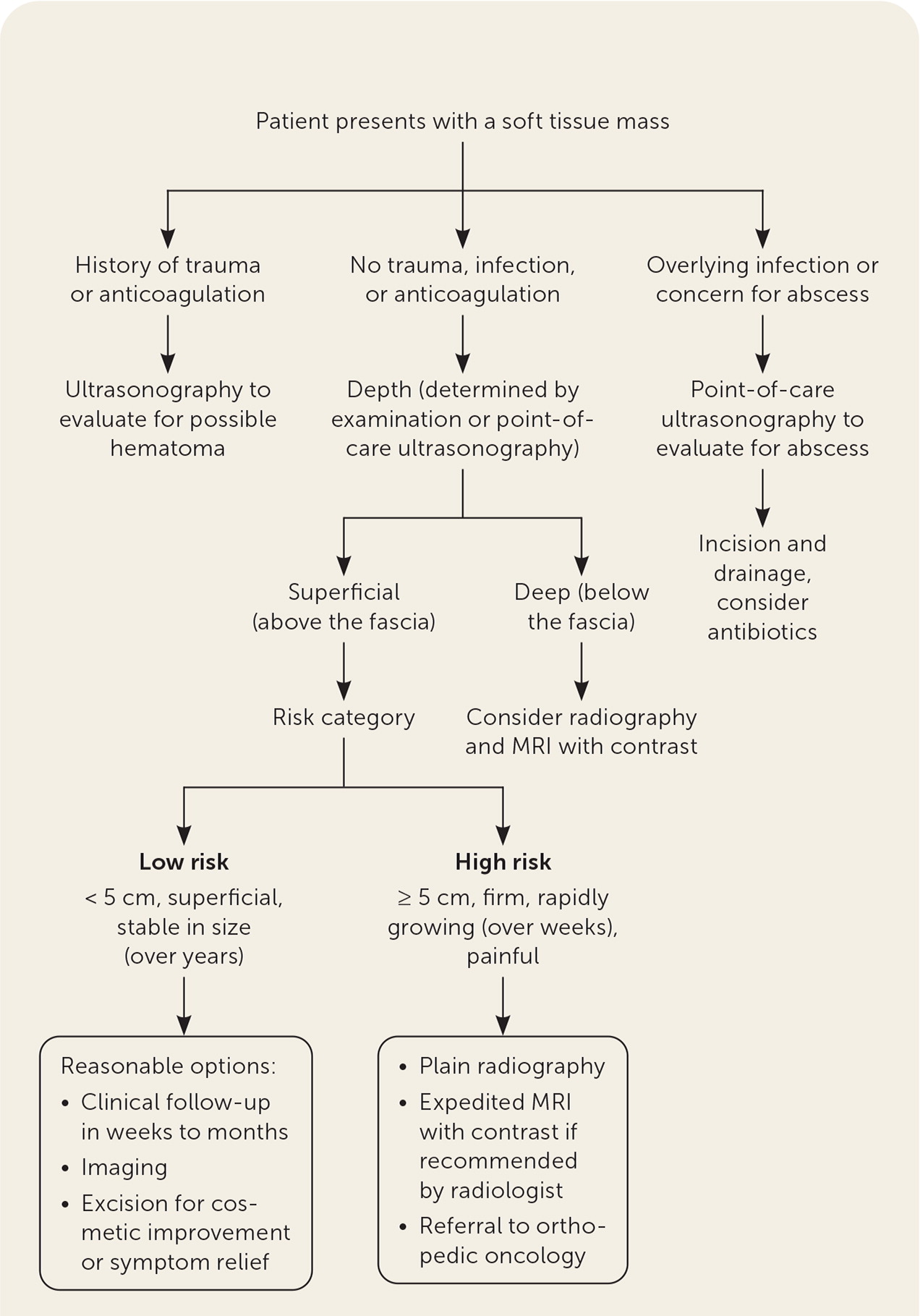
Soft tissue masses are a common presentation in family physician offices. Although most lesions, including lipomas, fibromas, and epidermal and ganglion cysts, are benign, rare lesions such as soft tissue sarcomas may have serious consequences. Masses that are deep to the fascia, are 5 cm in diameter or larger, grow rapidly, or present suddenly without explanation should prompt further workup. Imaging for concerning lesions may include ultrasonography, radiography, and sometimes magnetic resonance imaging with contrast. Ultrasonography can be used to assess size, depth, solid or cystic nature, and associated vasculature. Magnetic resonance imaging with contrast provides spatial orientation and delineation of soft tissue sarcomas from surrounding tissues such as muscles. Although less commonly used, computed tomography is an alternative in the initial evaluation of concerning masses and can assist with staging of retroperitoneal and visceral sarcomas. Incisional biopsy of a concerning soft tissue mass can also be useful for establishing a diagnosis. Lipomas and epidermal cysts may be excised if they are painful or if there is concern for malignancy. Because of the high mortality rate of soft tissue sarcomas, evaluation of high-risk masses with magnetic resonance imaging with contrast should be expedited with a referral to orthopedic oncology.
| Clinical recommendation | Evidence rating | Comments |
|---|---|---|
| Signs that increase the risk of malignancy include tumor size of 5 cm or larger, location on or below the fascia, masses matted to surrounding structures, and rapid growth.5 | C | Case series of patients referred with sarcoma |
| Point-of-care ultrasonography can be used to diagnosis abscesses.7 | A | Systematic review and meta-analysis |
| Consider initial imaging with radiography before more advanced imaging to evaluate for bony involvement and intratumoral calcifications in osteogenic or synoviosarcomas.55 | C | American College of Radiology guidelines |
| When a worrisome mass is found, initial radiography followed by an expedited MRI with contrast are recommended pending radiology recommendation and referral to an orthopedic oncologist.5,19,65 | B | Systematic review |
| Type | History | Examination | Imaging | Treatment |
|---|---|---|---|---|
| Abscess | Progressive, subcutaneous, erythematous swelling with possible drainage6 | Erythematous mass | Ultrasonography showing focal collection vs. “cobblestoning” with cellulitis7 | Incision and drainage with ultrasound guidance7 Consider antibiotics if recurrent or patient is immunocompromised8–10 |
| Epidermal inclusion cyst | Nodule under the skin11 | Arise in areas with hair follicles Pain and erythema if inflamed11 Mobile subcutaneous masses Hallmark feature is central punctate1,12 | MRI: well-defined T2 hyperintense lesions, may depend on presence of internal debris; ruptured cysts have a more varied appearance12 | For mildly inflamed epidermal inclusion cysts, incision and drainage with culture12 Can consider excision if recurrent11 |
| Ganglion cyst | Arises from joint, ligament, or tendon injuries13 | Most often on hands, wrists, feet, or ankles13,14 | Ultrasonography to distinguish between cystic and solid masses, locate adjacent blood vessels, and distinguish between other diagnoses, including a ruptured Baker cyst and deep venous thrombosis | Observation if no functional impairment15 Consider aspiration, steroid injection, or surgical excision if functional impairment or recurrent14,15 |
| Hemangiomas/arteriovenous malformations | Capillary hemangiomas are the most common type12,16 | Soft, compressible masses; diffuse blue or purple skin discoloration17 | Radiography and ultrasonography may reveal lesions containing phleboliths and mixed echogenicity MRI can demonstrate depth of the lesion16 | Conservative treatment can include observation or intravascular sclerotherapy17 Surgical referral reserved for patients with symptomatic tumors17* |
| Hematoma | Rapid onset Should have an explanation (e.g., anticoagulation, trauma) | Fluctuant mass, sometimes with overlying ecchymosis18 | Ultrasonography and MRI can show extent of the hematoma19 | Mainly conservative treatment; evaluate if persisting or enlarging for more than one month20 Consider embolization if progressively expanding21 |
| Intramuscular myxoma | Rare (0.12% of soft tissue tumors) Typically occurs in large skeletal muscles Most common between 40 and 70 years of age; slightly more common in women | Palpable mass, most common on the thigh and lower limb girdle22 | MRI: T1 hypointense to muscle, high signal intensity on T2-weighted or fluid-sensitive sequences | Surgical excision in most cases22 |
| Lipoma | Most common between 40 and 70 years of age and in patients who are obese16,23 Slightly more common in men24 Some genetic syndromes cause multiple lipomas | Superficial mass that is freely mobile with a doughy consistency24 Deep masses may involve muscle and move with muscle contraction24 | Radiographs may appear normal24 Ultrasonography: often isoechoic to adjacent subcutaneous fat24 MRI is required for any deep mass or subcutaneous lesion ≥ 5 cm24 MRI demonstrates fat signal intensity 24 | Monitoring for asymptomatic lipomas Consider excision for symptomatic or painful masses, or for cosmetic reasons24 |
| Lymphangioma: capillary, cavernous, or cystic | Appears at birth or by 2 years of age Pain is uncommon unless infection is present Disfigurement can be significant25 | Seen on the neck and axilla Soft on palpation Respiratory compromise is the most serious complication25 | Chest radiography may be useful in identifying mediastinal extension or pleural effusions Ultrasonography: hypoechoic, multilocular cystic masses25 CT: cystic lymphangioma; thicker septations are delineated | Observation only in the absence of symptoms Excision is the standard treatment Recurrence can be 27% and mortality about 2%25 Intralesional sclerotherapy is first-line treatment for macrocystic lymphangiomas26 |
| Morton neuroma (peripheral nerve sheath tumor)27 | Sensation of a “pebble in the shoe” or burning in toes distal to the neuroma27 | No visual clues to neuroma Mulder click test (dorsiflexing the foot and squeezing the metatarsals produces a clicking sound) | Radiography to rule out other sources of foot pain Ultrasonography can be used to identify a neuroma and guide injection MRI: neuroma seen on T1 axial slice28 | Wide toe box shoes Cortisone injections Surgical excision |
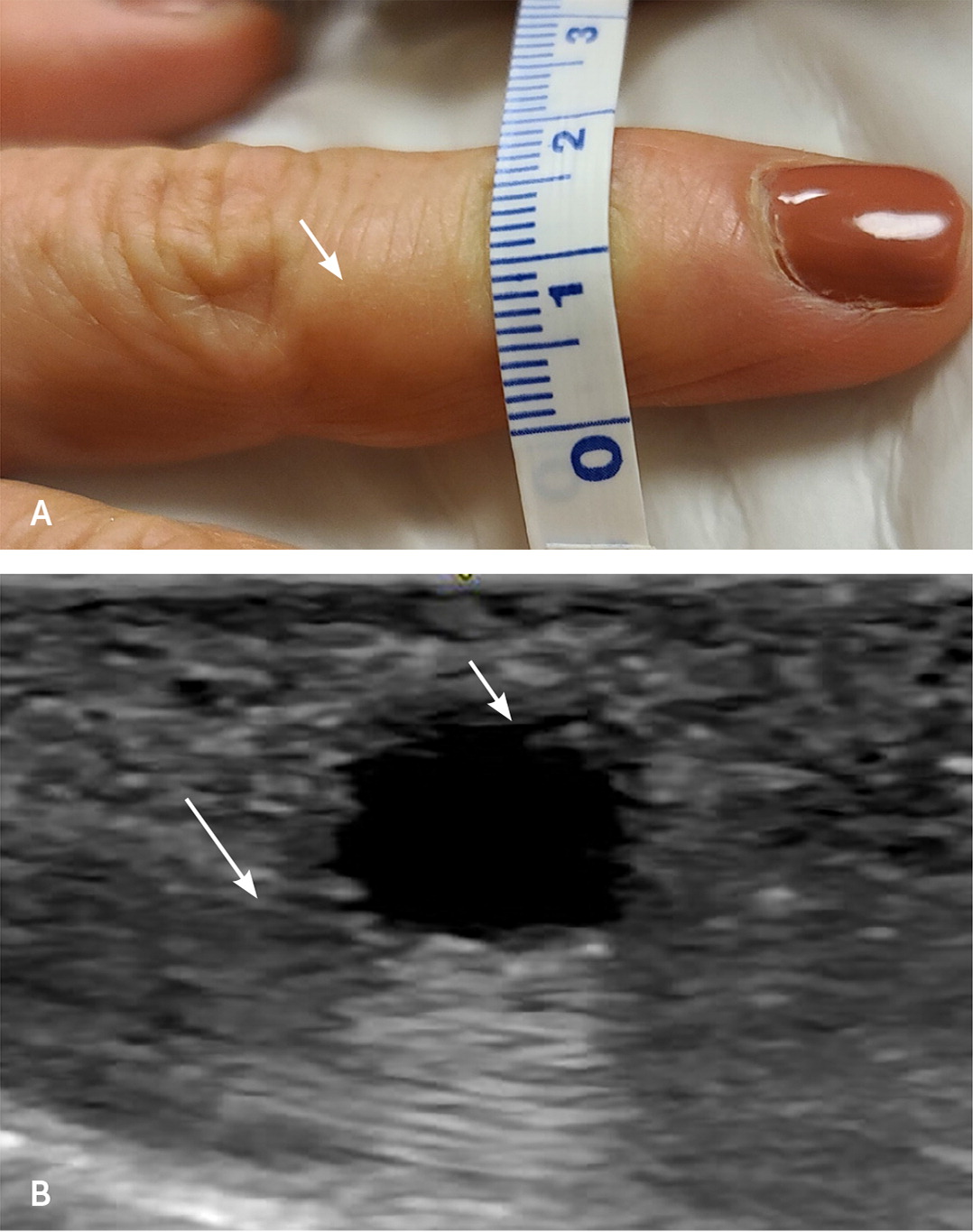
| Mucous cyst | Finger swelling, pain, tenderness, decreased range of motion 80% occur between 50 and 70 years of age29 Twice as likely in women than men29 Approximate prevalence: thumb 18%, second finger 26%, third finger 38%, fourth finger 9%, fifth finger 8%29 | Nail changes Translucent mass adjacent to the nail bed30 | Dermoscopic examination has reduced need for ultrasonography and radiography 30 | Surgical excision yielded the highest cure rate (mean of 95%) Second-line: sclerotherapy and cryotherapy Third-line: corticosteroid injections, expression of cyst content31 |
| Pilar cyst | 90% occur on the scalp32 Most common after 15 years of age Slightly more common in women32 | Swelling over the scalp Area of alopecia Well-defined, oval mass Occurs in areas with dense hair follicles32 | Imaging not usually warranted Ultrasonography: internal echogenic foci with demonstrated calcification, cholesterol crystals, or both; no blood flow in the lesion33 MRI: homogeneous, isointense signal on T1-weighted images; homogeneous, hyperintense signal on T2-weighted images32 CT: well-defined, hypodense masses with occasional calcification34 | If benign, treat with simple local excision If malignant, refer for wide local excision and possible Mohs surgery32 |
| Plantar fibroma | Mild pain that worsens after walking or standing for longer periods Bilateral in 20% to 50% of cases May have had trauma to the area or family history35 | Palpable nodule or focal thickening along the plantar fascia | Ultrasonography: fusiform nodules that are hypoechoic to isoechoic without intrinsic vascularity (comb sign)36 MRI: well-defined mass, isointense to muscle on T1-weighted images; well-defined, broad base at the superficial fascia demonstrates a fascial tail from extension of the tumor along the fascial plane | Can locally recur35 Orthotics Intralesional corticosteroid injection Consider subtotal fasciectomy with wide excision if conservative therapies are ineffective36 |
| Myositis ossificans | Common after trauma37 | Painful, rock-like mass Commonly affects quadriceps femoris and brachialis muscles Organized calcification within the muscle38 | MRI: classic hyperintense mass, calcifications may appear on T2-weighted images Radiography or CT: early detection with typical peripheral zonal ossification37 | Self-limiting with prolonged resolution common Consider referral for debilitating cases |
| Schwannoma in the foot | Swelling along the flexor surface Most common between 30 and 40 years of age Men and women affected equally39 Account for 5% of benign soft tissue tumors40 May present similarly to Morton neuroma | Clinical presentation depends on tumor size and location41 Motor or sensory disturbances along the flexor surface | Radiograph findings are often negative MRI shows lesions along a neurovascular bundle; a nerve may enter or exit a mass | Small asymptomatic tumors may be followed clinically If symptomatic, patient should be referred for biopsy with histologic examination and surgical excision41 |
| Tenosynovial giant cell tumor | Swelling most often in hands or feet Common between 30 and 50 years of age Slightly more common in women Second finger is most often affected42 | Rounded or lobulated mass appears to encase the surface of a tendon | Radiography: bony erosions Ultrasonography: small tumor with blood flow that does not attach to tendon MRI: lesion has low signal compared with muscle on T1-weighted images; hemosiderin deposition on T2-weighted images41 | Surgical resection Recurrence rate as high as 15%40 |
| Type | History | Examination | Imaging | Treatment |
|---|---|---|---|---|
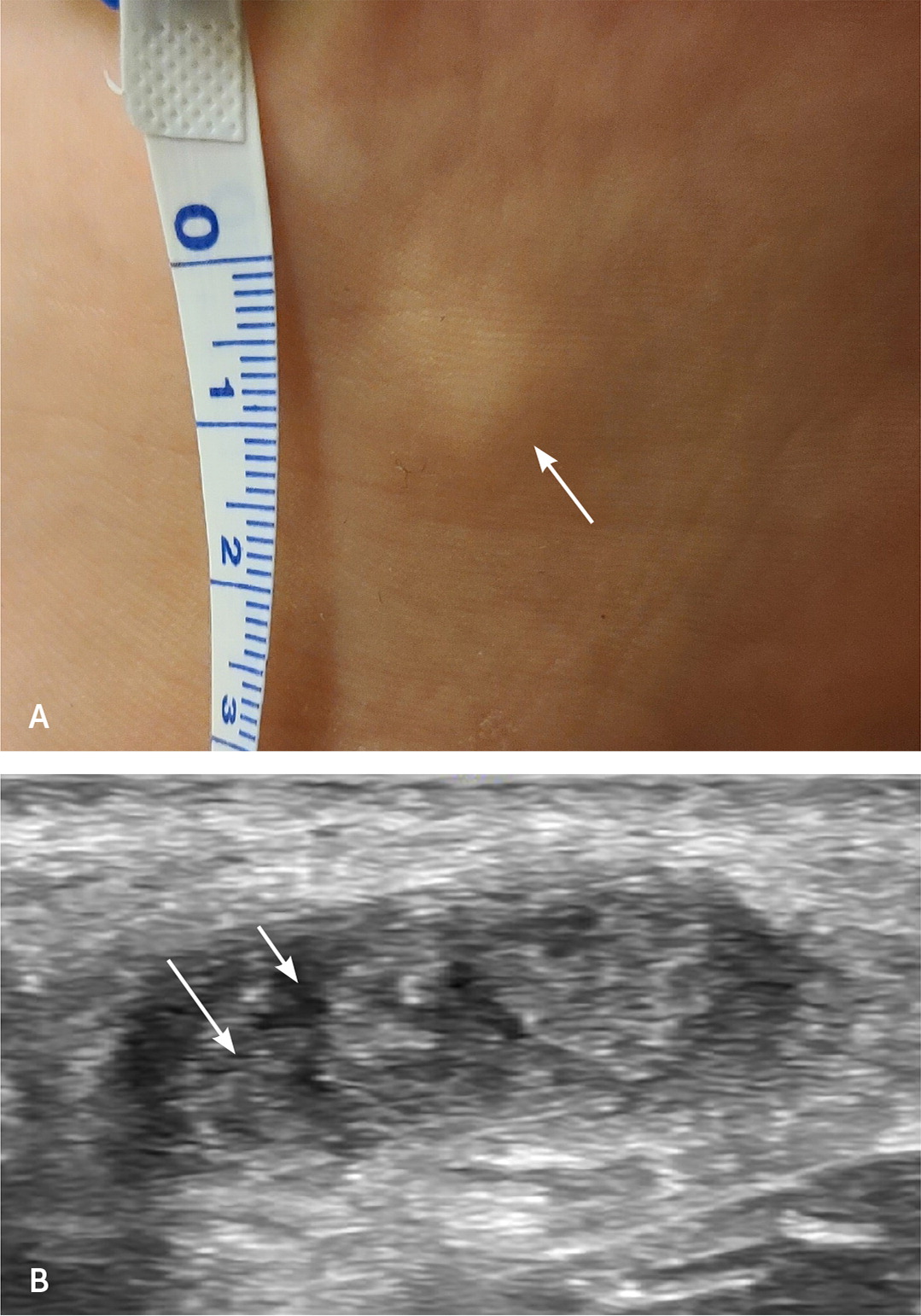
| Dermatofibrosarcoma protuberans | Median age of presentation is 20 to 59 years Equally common in men and women43 Lesion is slow-growing and present for years Account for 1% of all soft tissue sarcomas | Pink plaque44 Approximate prevalence of nodules: trunk 50% to 60%, upper limbs 25%, head and neck 10% to 15%44 Untreated lesions may ulcerate or bleed | Ultrasonography shows tentacle-like projections, hypervascularity45 MRI or CT is useful for recurrent disease or large and atypical primary lesions45 | Referral to orthopedic oncology for core needle biopsy and excision Wide excision with negative margins Mohs surgery for lesions that have wide margins or for cosmetic reasons43,44 |
| Leiomyosarcoma46,47 | Patients may report abdominal or back pain More common in adults older than 55 years In younger age groups, leiomyosarcoma is more common than liposarcoma | Enlarging mass on the limbs but can also occur on the head, neck, and retroperitoneum Palpable abdominal mass or symptoms of bowel obstruction46 | CT with contrast shows heterogeneous mass MRI can be used for patients with contrast allergies or for further investigation of muscle or bone involvement if equivocal on CT | Referral to orthopedic oncology for core needle biopsy and surgery46 |
| Liposarcoma | Accounts for about 17% of all soft tissue sarcomas48 Painless, rapidly enlarging soft tissue mass Most common between 50 and 60 years of age Equally common in men and women49 Rare in children; in young children, more likely to be lipoblastoma50 | Fullness or asymmetry, mobile unless attached to bone, nontender Lymph node examination is required | Radiography shows fat-attenuation or soft-tissue masses; calcifications or ossification in 10% to 32% of cases23 MRI findings can vary significantly depending on subtype and grade50,51 Large tumor size with thick septa and nodular or patchy nonadipose components are indicative of well-differentiated liposacromas51 | Referral to orthopedic oncology for core needle biopsy and resection |
| Rhabdomyosarcoma | Painful cervical mass Commonly seen in children younger than 10 years Rare in adults52 | Approximate prevalence: head and neck region near orbit 40%, urinary or reproductive organs 30%, extremities 15%, other locations 15%47 | Ultrasonography is the first-line imaging study for investigating soft tissue masses in children34 Imaging findings vary depending on location | Referral to orthopedic oncology |
| Synoviosarcoma | Slow growing Most common in adults 30 to 40 years of age16,47 | Mass size typically between 3 cm and 10 cm May be painful | Radiography shows calcification in 33% of cases35 Ultrasonography: heterogeneous mass with areas of necrosis and eccentric calcifications with variable vascularity47 MRI: well-demarcated mass, isointense to muscle on T1-weighted images47 Extrinsic bone erosion in 11% to 20% of cases | Diagnosis can be delayed because of slow growth Referral to orthopedic oncology for core needle biopsy and resection |
History and Physical Examination
Malignant masses may grow over weeks to years depending on the aggressiveness of the tumor.5 Both benign and malignant masses can be painless, but those that present suddenly without explanation or are firm, deep, and adhere to surrounding structures are more concerning for malignancy.5 Sarcomas do not fluctuate in size, whereas masses such as hemangiomas and ganglion cysts often do.
Based on strong evidence, lesions that are 5 cm in diameter or larger should be evaluated with advanced imaging or the patient referred because of a higher risk of malignancy.5,52 However, smaller size does not exclude malignancy because approximately 10% of malignant soft tissue masses are smaller than 5 cm when diagnosed.53 Because of the high mortality rate of soft tissue sarcomas and the potential to miss a small sarcoma, any mass that is not definitively diagnosed should be closely monitored or the patient referred to orthopedic oncology.5
Examination includes inspection of the skin and palpation of the mass to assess its depth, mobility, and adherence to deeper structures. Measurement can be difficult, but using a 4- to 5-cm golf ball as a reference can be helpful.
| Biopsy https://www.aafp.org/fpm/2019/0300/p15.html |
| Ganglion cyst aspiration https://www.aafp.org/afp/2003/0215/p745.html |
| Point-of-care ultrasonography https://www.aafp.org/fpm/2020/1100/p33.html |
Imaging Studies
ULTRASONOGRAPHY
RADIOGRAPHY
The accuracy of plain radiography for diagnosing soft tissue tumors is limited. Radiography should be considered before advanced imaging to evaluate for bony involvement and intratumoral calcifications in osteogenic or synoviosarcomas.55
MAGNETIC RESONANCE IMAGING
COMPUTED TOMOGRAPHY
Biopsy
Laboratory Studies
Sarcomas
Soft tissue sarcomas are a broad and heterogenous group of tumors that are most common in adults older than 55 years, although they can occur at any age.60 Malignancy in children is rare; however, sarcomas represent up to 15% of childhood malignancies, 60% of which occur in the extremities.61 Family physicians should be vigilant because patients with sarcomas have a high mortality rate and often do not seek care right away. Nearly one-half of patients diagnosed with sarcomas wait at least one month from recognition of the mass to see a health care professional.61
Common Soft Tissue Masses
ABSCESS
Skin and soft tissue abscesses are common, with increasing incidence.66 They can present anywhere on the body but are more often found at sites of skin damage.66 Risk factors for progression from cellulitis to abscess include delay in treatment, male sex, smoking, and alcoholism.6 Point-of-care ultrasonography is more accurate than clinical examination for diagnosing abscesses and can assess exact size, depth, and presence of loculi within the abscess.7 In addition to characterizing an abscess, ultrasonography can guide incision and drainage procedures.67
LIPOMA
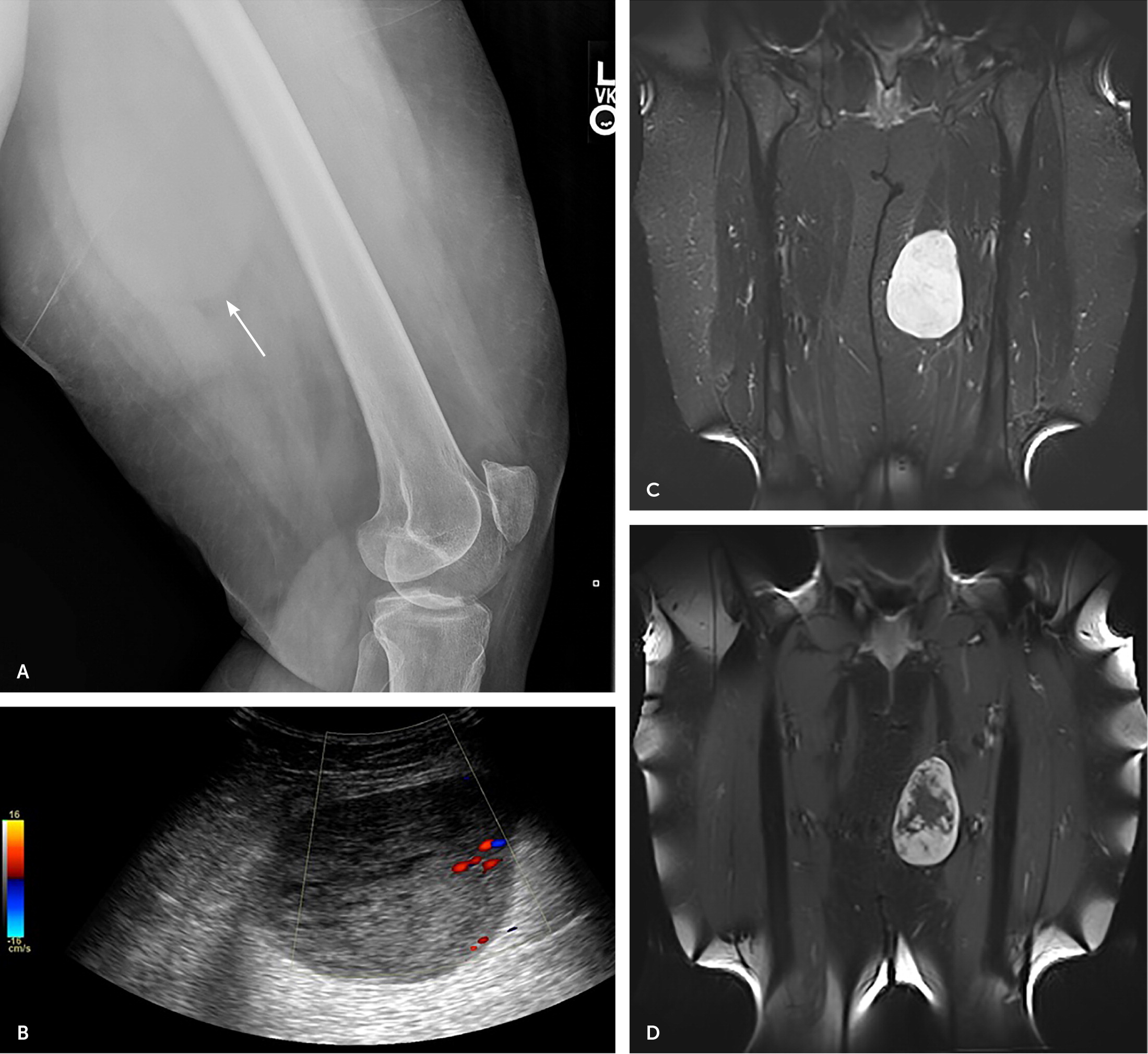
Lipomas are soft, fatty deposits (Figure 3) that account for approximately one-half of benign soft tissue masses.1,16,23,50,68–70 Lipomas can develop at any age, with a predilection for the trunk and proximal extremities, although they are most common in patients who are 40 to 70 years of age or obese.16,23 Presentation in children is often varied and nonspecific, and lesions can grow rapidly during periods of weight gain.50 Patients who have family members with multiple lipomas may have a genetic condition called familial multiple lipomatosis, which presents with multiple benign lipomas on the extremities or trunk.23 Because some lipomas are deep to the fascia, they can be larger than what is felt on palpation.
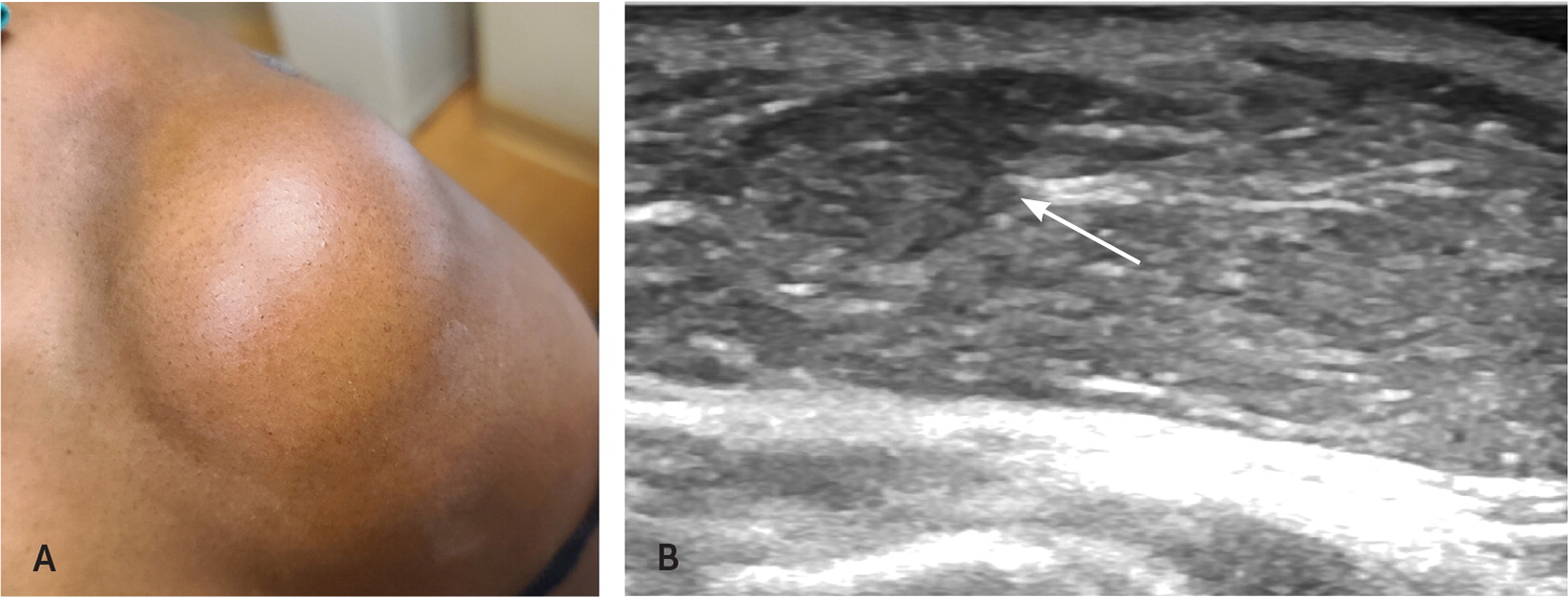
Common lipoma characteristics visible on ultrasonography include an elongated and well-circumscribed solid mass that may contain a fibrous capsule (Figure 3B). Approximately one-third of benign lipomas may also contain fatty necrosis with calcifications, making a benign lipoma difficult to differentiate from the rare liposarcoma.69,71
EPIDERMAL INCLUSION CYST/PILAR CYST
Epidermal inclusion cysts, also called epidermoid cysts and formerly called sebaceous cysts, are dome-shaped masses that arise in areas with hair follicles. These masses contain keratin debris and are encapsulated by a wall of stratified squamous epithelium, with a hallmark central punctum on the skin.1,12 Epidermal inclusion cysts can present as mobile subcutaneous masses that are as small as a few millimeters to 5 cm in diameter.1 Multiple epidermal inclusion cysts can be associated with Gardner syndrome.59
A rapidly growing epidermal inclusion cyst or recurrence after surgical excision warrants further investigation for malignancy. Epidermal inclusion cysts should be removed en bloc because they can recur if not completely removed. Ruptured cysts may become infected and often require antibiotic treatment.15,59
GANGLION CYST
BAKER CYST
PLANTAR FIBROMA
Patients often present with a painful nodular lesion in the midsubstance or superficial aspect of the plantar fascia that is worsened with walking or standing. Plantar fibromas are bilateral in 20% to 50% of cases.35 Examination may reveal a focal thickening along the plantar fascia or a palpable nodule.36 On ultrasonography, plantar fibromas appear as fusiform nodules that are hypoechoic to isoechoic without intrinsic vascularity (comb sign).5,36
Treatment rarely requires excision, and many plantar fibromas can be managed conservatively with shoe padding or modifications. Corticosteroid injections (under ultrasound guidance if possible) can relieve pain and decrease the size of the fibroma.36,72 If orthotics and intralesional corticosteroid injections are ineffective, a subtotal fasciectomy with wide excision can be considered.36
Data Sources: Essential Evidence Plus, PubMed, the Cochrane database, and Scopus were searched using the terms soft tissue masses, sarcoma, cyst, ganglion cyst, plantar fibroma, vascular lesions, epidermal cyst, and pilar cyst. Search dates: February 2021 to March 2022.
