
Am Fam Physician. 2022;106(1):27-35
Related Letter to the Editor: Additional Considerations for the Microscopic Evaluation of Urine
Author disclosure: No relevant financial relationships.
Comprehensive urinalysis involves inspection of the urine, dipstick chemical analysis, and microscopy and can be performed in the office setting. When testing for urinary tract infection, midstream urine should be collected using the clean-catch technique. A urine collection bag specimen can be used for clinically stable febrile infants with suspected urinary tract infection; however, the presence of leukocyte esterase or nitrites warrants more invasive urine collection. Urine specific gravity shows hydration status. Urinary pH levels can indicate diet, metabolism, or the presence of stones. Bilirubin and urobilinogen may suggest hepatobiliary disease or hemolysis. Glucosuria often indicates uncontrolled diabetes mellitus, and ketones suggest illness and inadequate nutrition. Hematuria on dipstick testing can be confirmed in the office using a spun urine sample. Proteinuria on dipstick testing should be followed by a quantitative test such as a spot urine albumin/creatinine ratio. In patients with symptoms of a urinary tract infection, the presence of nitrites is more specific for bacterial infection, and a positive leukocyte esterase result may occur from inflammation and infection. Asymptomatic bacteriuria is often unnecessarily treated in older patients. Without symptoms of urinary tract infection, urine culture is useful only in pregnancy and preparation for endoscopic urologic procedures.
Urinalysis is a simple, inexpensive means of detecting urologic and systemic conditions such as infection, urolithiasis, malignancy, and metabolic diseases. Urinalysis can be outsourced or performed in the office by clinical staff. Familiarity with a visual inspection of the urine, dipstick testing, and point-of-care microscopy is an important diagnostic skill for family physicians. This article reviews and updates the practical use of office-based urinalysis and the differential diagnosis for abnormal results.
| Clinical recommendation | Evidence rating | Comments |
|---|---|---|
| In infants and children, the presence of leukocyte esterase or nitrites in a urine collection bag urinalysis requires follow-up urinalysis using clean urine collection by urethral catheterization or suprapubic aspiration.8 | C | Expert opinion |
| Urinary pH should be assessed in patients with urolithiasis to help determine the type of stone.14 | C | Expert opinion |
| Proteinuria on dipstick testing should be followed up with a quantitative test such as a spot urine albumin/creatinine ratio.18 | C | Guideline based on expert opinion |
| The presence of nitrites in the urine of a patient who is symptomatic strongly suggests a UTI; however, the absence of nitrites does not eliminate the possibility of a UTI.6,12,15 | C | Consistent, good-quality studies |
| Dipstick testing positive for blood should be confirmed with microscopic analysis.5 | C | Guideline based on consistent, good-quality studies |
| Recommendation | Sponsoring organization |
|---|---|
| Do not diagnose microhematuria based only on the results of one urine dipstick test (macroscopic urinalysis). | American Urological Association |
| Do not initiate a workup for hematuria or proteinuria before repeating an abnormal urine dipstick analysis. | American Academy of Pediatrics – Section on Nephrology and the American Society of Pediatric Nephrology |
| Do not order screening urinalysis in healthy, asymptomatic children as part of routine well-child examinations. | American Academy of Pediatrics – Section on Nephrology and the American Society of Pediatric Nephrology |
Setting Up In-Office Urinalysis
Urine dipstick test kits are widely available and easy to use. Results may be interpreted visually off the dipstick or by an automated machine.1 Microscopic analysis requires a centrifuge and microscope, with commonly used 10×, 40×, and 100× (oil immersion) objectives. Phase-contrast and polarized microscopes help identify casts and crystals, respectively, but are not commonly used in office settings.2
The Clinical Laboratory Improvement Amendments (CLIA) regulate medical testing, and dipstick urinalysis can be performed in a physician’s office by obtaining a CLIA certificate of waiver. Clinician-performed microscopy is considered moderate complexity testing and requires a demonstration of quality assurance by proficiency testing or split sampling.2 The American Academy of Family Physicians has published detailed guidance for navigating this process.3
Specimen Collection
The American Society for Microbiology recommends midstream urine collection with genital cleansing when possible, regardless of age and sex, despite a lack of evidence that this strategy decreases contamination.4 The American Urological Association also recommends midstream collection for evaluation of microhematuria.5 Urine should be refrigerated or tested promptly after collection to avoid incorrect results.6
In clinically stable infants and children, the initial urinalysis can be performed using a convenient collection method, such as a urine collection bag specimen. Urine culture of a bag specimen is not recommended. Alternatively, successful midstream urine collection has been described using suprapubic and lumbosacral stimulation, such as the Quick-Wee approach.7 If urinalysis shows the presence of leukocyte esterase or nitrites, follow-up urinalysis using clean urine collection by urethral catheterization or suprapubic aspiration should be performed.8 An online risk calculator can help in the assessment of urinary tract infection (UTI) in infants (https://uticalc.pitt.edu).
Visual Appearance and Odor
The yellow color of urine is caused by urochrome generated from the breakdown of hemoglobin. Foods, drugs, metabolic products, and infections can cause an abnormal urine appearance (Table 1).6,9–11 Cloudy urine suggests an infection (positive likelihood ratio = 3) but can indicate alkaline urine with precipitated phosphate crystals.6,12 Gross hematuria is concerning for malignancy. Visible feces in the urine can suggest an enterovesical fistula, whereas nonfeculent brown urine may indicate ingestion of fava beans. Fluorescence by Wood lamp can demonstrate porphyrins in heme biosynthesis disorders. Purple urine bag syndrome can occur in patients with long-term indwelling catheters because of metabolites from certain types of bacterial overgrowth (Figure 1).11
| Appearance | Physiologic/pathologic | Food/drug/herb related |
|---|---|---|
| Brownish-black | Bile pigments, copper poisoning, melanin, methemoglobin, myoglobin, porphyria, stool from fistula | Aloe, cascara sagrada or senna (bitterbark), fava beans, levodopa, methocarbamol (Robaxin), methyldopa, metronidazole (Flagyl), nitrofurantoin, some antimalarial agents, sorbitol |
| Cloudy or white | Chyle, infection, lipids, oxalates, phosphates | Propofol (Diprivan), purine-rich foods (hyperuricosuria) |
| Foamy | Dehydration, frank proteinuria | — |
| Green or blue | Biliverdin, pseudomonas | Amitriptyline, cimetidine (Tagamet), indigo carmine (diagnostic agent), indomethacin, methylene blue (ProvayBlue; methemoglobin treatment), prochlorperazine, propofol, triamterene (Dyrenium) |
| Orange | Bile pigments, uric acid in newborns | Carrots, phenazopyridine, rifampin, sulfasalazine (Azulfidine) |
| Purple | Bacterial overgrowth from indwelling catheter | — |
| Red | Hematuria, hemoglobinuria, myoglobinuria | Beets, blackberries, phenothiazines, phenytoin (Dilantin), rhubarb, senna |

Dehydration leads to concentrated, strong-smelling urine. A fruity or sweet odor can indicate diabetic ketoacidosis. Foul smells such as ammonia can indicate a UTI or an infected kidney stone. Although a feculent odor suggests a fistula, a sulfur-like odor can be attributed to ingestion of a sulfa medication or asparagus.6
Dipstick Urinalysis
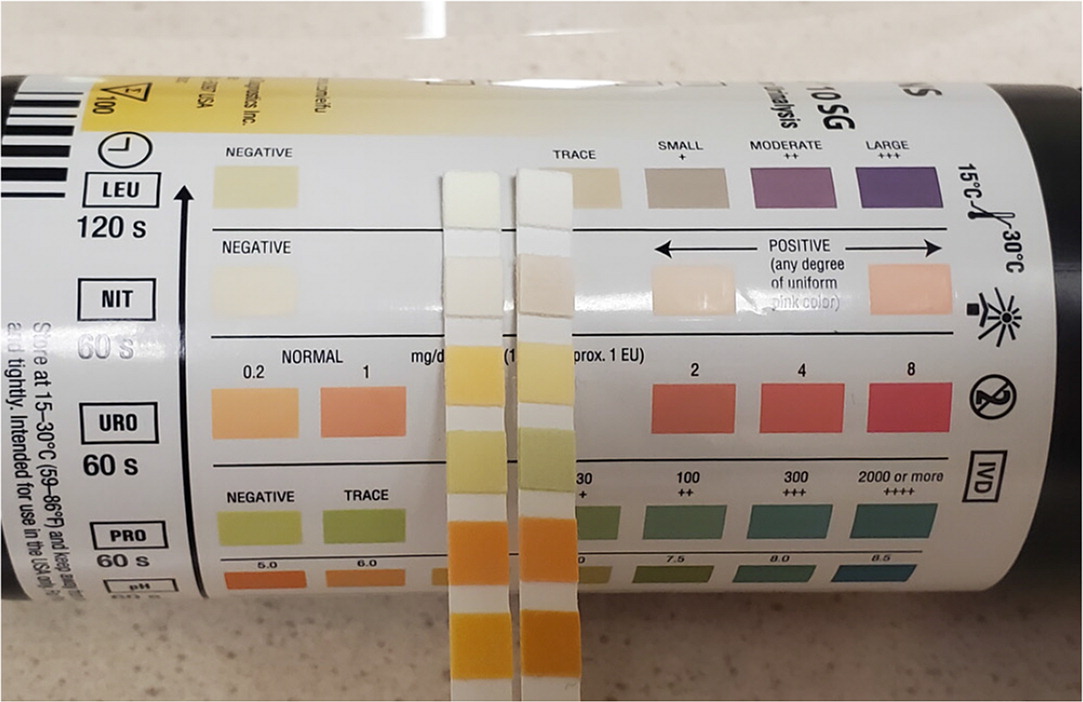
Dipsticks visually display results after a sufficient time in contact with urine. The color change is compared with a reference standard to determine the concentration of the analyte being measured.1 The dipstick result is usually read after 60 to 120 seconds. The leukocyte esterase dipstick test is the most sensitive to time. Substances and medical conditions can also affect dipstick results. Nitrite results can be inaccurate when the dipstick is left unpackaged in the open air (Figure 2).
| Dipstick test result | Suggested diagnoses | False-positive results | False-negative results |
|---|---|---|---|
| Bilirubin | Biliary obstruction, hepatic disease | Chlorpromazine, phenazopyridine | Prolonged light exposure, selenium, vitamin C |
| Blood | Glomerular disorders, hypercalciuria, hyperuricosuria, kidney stones, trauma, tubular disorders, tumor, UTI | Exercise, hemoglobinuria, menses, myoglobinuria | High urine specific gravity, vitamin C |
| Glucose | Diabetes mellitus, Fanconi syndrome, pregnancy, sodium-glucose cotransporter-2 inhibitor use | Levodopa, strong oxidizing agents | High pH, high urine specific gravity, uric acid, vitamin C |
| Ketones | Diabetes, ketogenic diet, pregnancy, starvation | High urine specific gravity, low pH, some drug metabolites | Delay in examination of urine;certain ketones not detectable depending on brand of test |
| Leukocyte esterase | Inflammatory process, sexually transmitted infection, UTI | Contamination | Antibiotics; high glucose, protein, or urine specific gravity; vitamin C |
| Nitrites | UTI | Contamination, dipstick exposure to air, phenazopyridine | High urine specific gravity, bacteria that do not reduce nitrates, short bladder incubation time, vitamin C |
| pH | High: alkalemia, carbonic anhydrase inhibitors, heavy antacid use, potassium/sodium citrate, type 1 renal tubular acidosis, UTI Low: acidemia, methenamine | — | Presence of formaldehyde |
| Protein | Fever, glomerular disorders, tubular disorders, UTI | Phenazopyridine, concentrated or alkaline urine, quaternary ammonium compounds | Nonalbumin proteinuria, acidic or diluted urine |
| Urine specific gravity | High: dehydration, glucosuria, syndrome of inappropriate antidiuretic hormone Low: adrenal insufficiency, aldosteronism, diabetes insipidus, impaired renal function, water intoxication | Dextran solutions, intravenous radiopaque dyes, phenazopyridine, proteinuria | Alkaline urine |
| Urobilinogen | Intravascular hemolysis, hepatic disease, sometimes a normal finding | Phenazopyridine, sulfonamides | Improper storage of the urine sample, preservatives |
| Findings for diagnosing UTI | LR+ |
| Positive nitrites | 13 |
| Positive blood | 3 |
| Cloudy appearance | 3 |
| Any white blood cells | 2 |
| Red blood cells > 5 per high-power field | 2 |
| Any bacteria | 2 |
| Findings for eliminating UTI | LR− |
| Negative leukocyte esterase, nitrites, and blood combined | 0.1 |
| No white blood cells | 0.1 |
| Negative leukocyte esterase and nitrites combined | 0.2 |
| Negative blood | 0.2 |
| No bacteria | 0.3 |
URINE SPECIFIC GRAVITY
The urine specific gravity shows concentrations of dissolved substances in the urine (osmolality). Dipstick urine specific gravity indicates only current hydration status. A value near 1.010 suggests euvolemia. A value exceeding 1.020 may indicate dehydration, glucosuria, or syndrome of inappropriate antidiuretic hormone. A value less than 1.003 suggests significant urinary dilution from diabetes insipidus, water intoxication, impaired renal function, adrenal insufficiency, or aldosteronism.6,13,16
URINARY PH
The urinary pH may vary from 4.5 to 8, but it is often between 5.5 and 6.5 because of excreted acids from renal metabolic activity. A high pH may be due to a high citrate diet, type 1 renal tubular acidosis, or infection with urease-positive bacteria such as Proteus. A low pH can occur with diets high in protein and acidic fruits.6,13 In patients with urolithiasis, the urinary pH can indicate the type of stone.14 A low pH occurs with uric acid, cystine, and calcium oxalate stones, and a high pH occurs with calcium phosphate and infected struvite/staghorn stones.14
BILIRUBIN AND UROBILINOGEN
Although unconjugated bilirubin is insoluble in water, conjugated bilirubin is soluble and can be excreted in urine. The presence of conjugated bilirubin on dipstick testing should prompt investigation for hepatobiliary disease. Urobilinogen is produced by the breakdown of bilirubin in the intestines. A trace amount of urobilinogen is often excreted in the urine; however, elevated levels on dipstick testing may indicate hemolysis or hepatic disease.6
GLUCOSE
The sodium-glucose cotransporter-2 (SGLT-2) in the proximal renal tubule normally reabsorbs glucose that passes through the glomerulus. When plasma glucose concentrations exceed 180 to 200 mg per dL (9.99 to 11.10 mmol per L), the transporters are overwhelmed, resulting in glucosuria. SGLT-2 inhibitors used for the treatment of type 2 diabetes mellitus can also cause glucosuria.17 Glucosuria without serum glucose elevations or SGLT-2 inhibitor use can be due to Fanconi syndrome, which is a rare disorder of the proximal tubule that leads to multiple electrolyte abnormalities.13
KETONES
Ketones are not normally found in urine. The presence of ketones can be attributed to increased fatty acid catabolism from inadequate nutrition, diabetic ketoacidosis, a ketogenic diet, and sometimes pregnancy.6
PROTEIN
Dipstick tests detect many proteins but are most sensitive to albumin (Table 4).6 A protein finding of 1+ or greater suggests glomerular injury.6 Dipstick testing that shows proteinuria should be followed by a quantitative test such as a spot urine albumin/creatinine ratio.18 A 24-hour urine collection is more cumbersome and subject to collection errors.
| Finding | Approximate proteinuria equivalent (mg per dL) |
|---|---|
| Trace | 5 to 10 |
| 1+ | 30 |
| 2+ | 100 |
| 3+ | 300 |
| 4+ | 1,000 |
The differential diagnosis for proteinuria is broad (Table 5).6,10 Proteinuria may be transient or persistent, and the source can be glomerular, tubular, or overflow. Benign causes of transient proteinuria such as orthostasis or exercise are common in asymptomatic patients, and the proteinuria may be resolved on repeat testing in the morning. Urine dipstick testing may not detect low-molecular-weight proteins such as light chain fragments in multiple myeloma (i.e., Bence Jones proteins).
| Transient Dehydration Exercise Fever Malignant hypertension Orthostatic proteinuria Preeclampsia Seizure Stress Primary glomerular Focal segmental glomerulosclerosis Immunoglobulin A or IgM nephropathy Membranoproliferative glomerulonephritis Membranous nephropathy Minimal change disease | Secondary glomerular Allergic (e.g., antitoxins, poison ivy or oak, stings, venomous bites) Collagen vascular diseases (e.g., IgA vasculitis, Sjögren syndrome, systemic lupus nephritis) Drugs (e.g., contrast media, heroin, lithium, NSAIDs) Genetic (e.g., Alport syndrome, Fabry disease, sickle cell disease) Infection (e.g., hepatitis B and C, HIV, malaria, poststreptococcal, syphilis) Metabolic (e.g., amyloidosis, diabetes mellitus, thyroid disease) Neoplastic (e.g., carcinomas, leukemia/lymphoma, multiple myeloma) | Tubular (typically nonalbumin dominant, < 2 g per day) Acute tubular necrosis Drugs (e.g., lithium, NSAIDs) Fanconi syndrome Heavy metals (e.g., copper, lead, mercury) Renal transplant rejection Tubulointerstitial nephritis Overflow disorders Hemoglobinuria Multiple myeloma Myoglobinuria |
LEUKOCYTE ESTERASE AND NITRITES
Leukocyte esterase and nitrites found on dipstick testing suggest a UTI. Leukocyte esterase is produced by neutrophils and may be present with inflammatory processes and infections.6,13 In one study of 705 children with culture-confirmed UTI, 71% of patients were positive for leukocyte esterase; however, this percentage decreased to 44% in patients with Enterococcus or Klebsiella infection.19
Nitrites are created by nitrate-reducing bacteria, and their presence has a higher specificity than leukocyte esterase for detecting a UTI.20 A few bacteria such as Enterococcus do not produce nitrites, leading to false-negative results.21 Bacteria need four hours in the bladder to produce nitrites; therefore, false-negative results are common with frequent urination, including in infants.13
BLOOD
Dipstick testing for blood detects peroxidase activity of red blood cells (RBCs) in the urine. These tests have a greater than 90% sensitivity for hematuria, but free hemoglobin and myoglobin can lead to false-positive results.6,22 Microscopic analysis is the best way to confirm dipstick testing positive for blood.5 Hematuria can be due to glomerular or nonglomerular causes6,23,24 (Table 623).
| Glomerular causes Familial Fabry disease Hereditary nephritis (Alport syndrome) Nail-patella syndrome Thin basement membrane nephropathy Primary glomerulonephritis Focal segmental glomerulonephritis Goodpasture syndrome Henoch-Schönlein purpura Immunoglobulin A nephropathy (Berger disease) Mesangial proliferative glomerulonephritis Postinfectious glomerulonephritis Rapidly progressive glomerulonephritis Secondary glomerulonephritis Hemolytic uremic syndrome Systemic lupus nephritis Thrombotic thrombocytopenic purpura Vasculitis | Renal causes Arteriovenous malformation Hypercalciuria Hyperuricosuria Loin pain–hematuria syndrome Malignant hypertension Medullary sponge kidney Metabolic causes Polycystic kidney disease Renal artery embolism Renal papillary necrosis Renal vein thrombosis Sickle cell disease or trait Tubulointerstitial cause Vascular cause | Urologic causes Benign prostatic hyperplasia Cancer (bladder, kidney, prostate, ureteral, or urethral) Cystitis/pyelonephritis Nephrolithiasis Prostatitis Schistosoma haematobium infection Tuberculosis Other causes Drugs (e.g., cyclophosphamide, heparin, nonsteroidal anti-inflammatory drugs, warfarin) Trauma (e.g., contact sports, running, Foley catheter) |
Microscopic Urinalysis
Microscopic examination of the urine in the office setting can confirm the presence of RBCs, white blood cells (WBCs), epithelial cells, and bacteria. Preparation for microscopy generally involves centrifuging 10 mL of urine for five minutes at 1,500 rpm or greater. After the clinician gently pours out the supernatant, the pellet is resuspended using a small amount of the leftover supernatant. A drop is placed on a clean slide with a coverslip and observed under low- and then high-power magnification while ensuring the field of view is representative.6,13,24,25
RED BLOOD CELLS
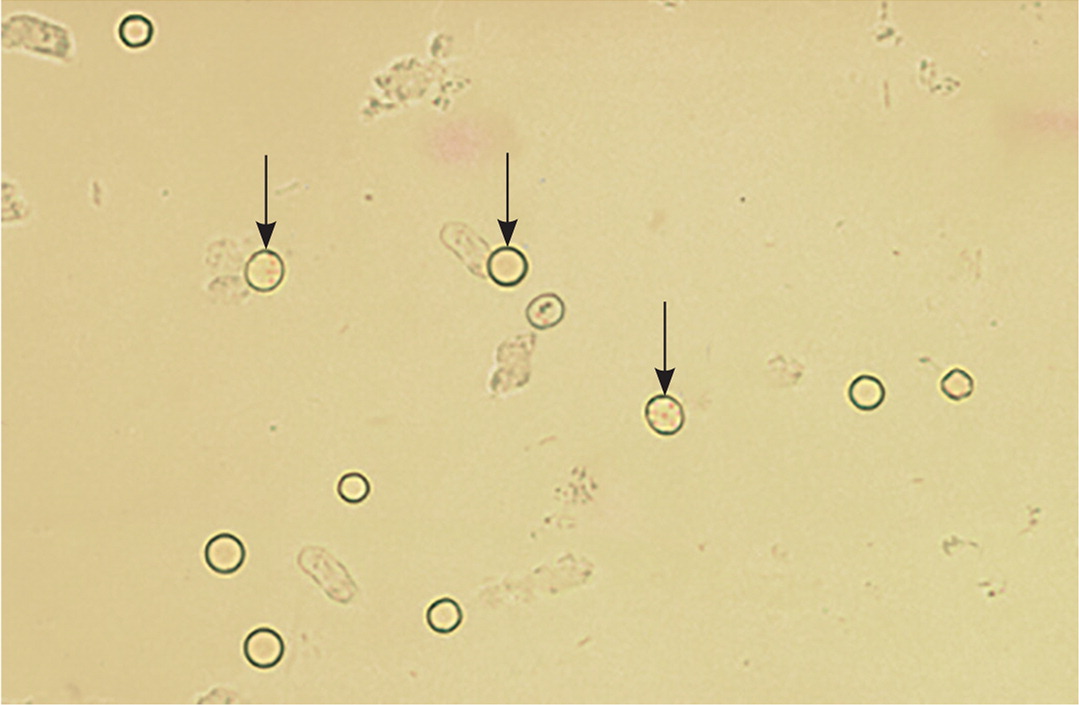
Microhematuria in adults is defined as three or more RBCs per high-power field on spun urine. In children, microhematuria is diagnosed with more than five RBCs per high-power field.5,24,26 The risk of genitourinary malignancy is 3% in patients with microhematuria; therefore, cystoscopy and imaging are recommended in intermediate- and high-risk adults in the absence of a clear nonmalignant cause. Cystoscopy should be considered for adults at low risk with continued microhematuria, especially if a benign cause such as exercise, menses, or UTI has resolved.5
WHITE BLOOD CELLS
Neutrophils are the most common WBCs found in urine. On microscopy, neutrophils are larger than RBCs and contain nuclei. Neutrophils can be found in infectious and inflammatory processes, including UTIs, sexually transmitted infections, and urolithiasis.6 More than five WBCs per high-power field is consistent with UTI for patients who are symptomatic (Figure 4). A portion of the urine sample may be tested for sexually transmitted infections via nucleic acid amplification, and a first morning void sample without cleansing detects sexually transmitted infections better than the midstream clean-catch samples recommended for diagnosing UTI.27 Urolithiasis should be suspected in patients with urinary WBCs and severe pain, RBCs, and urine crystals.
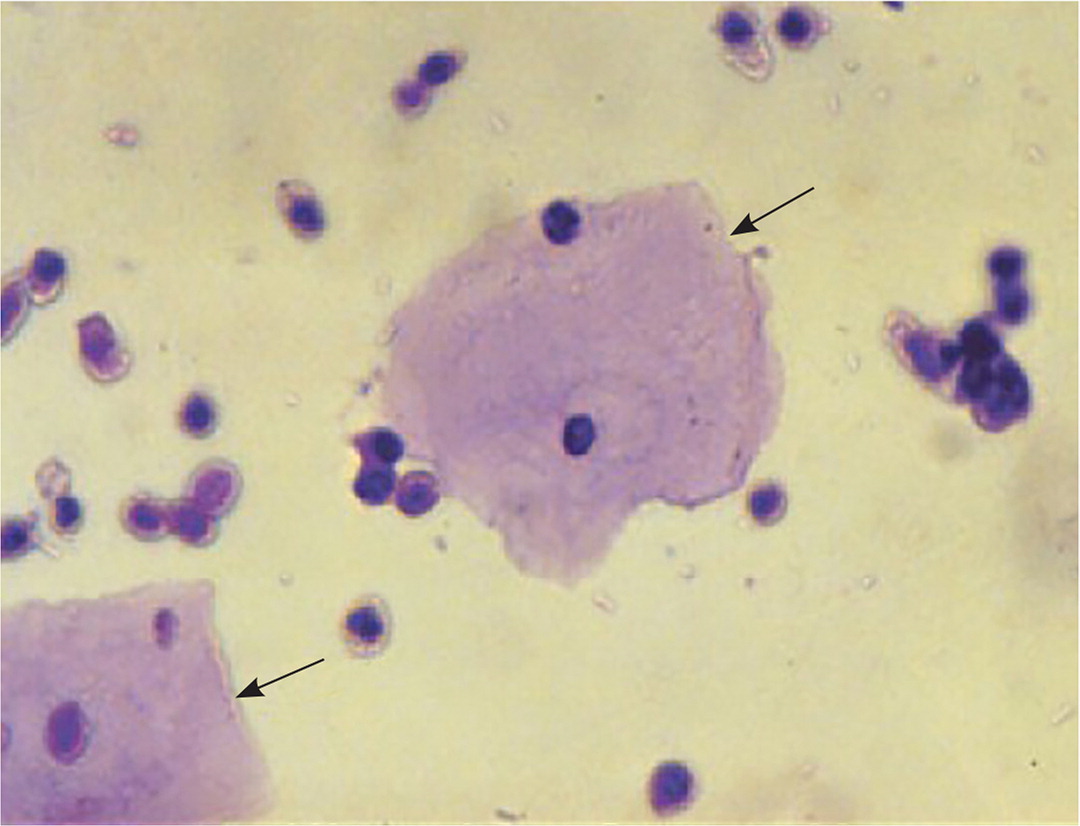
EPITHELIAL CELLS
BACTERIA
Bacteria are difficult to see on microscopy unless abundant. Bacteria may be present with infection and contamination. A urine culture is required to evaluate for a dominant bacterial species (Table 7).20,28–30 The presence of five bacteria per high-power field suggests that colony counts of 100,000 per mL will be found on urine culture.31 Urine culture is recommended when UTI symptoms are present. Screening for asymptomatic bacteriuria is recommended only in pregnancy and before endoscopic urologic procedures.32 Asymptomatic bacteriuria is often unnecessarily treated in older patients.
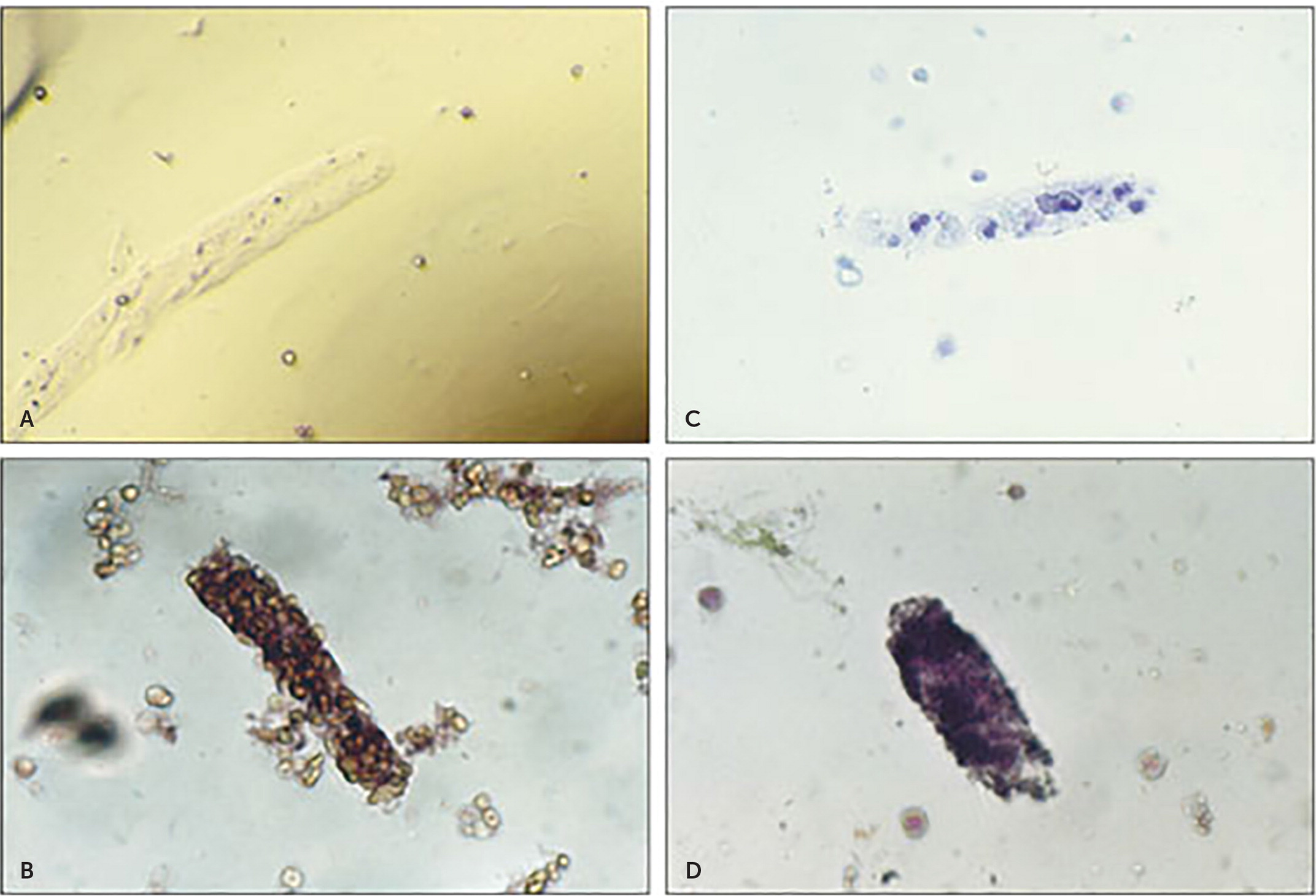
CRYSTALS AND CASTS
Although most urinary crystals can be viewed with normal microscopy, some are better viewed with polarized microscopy (eFigure A). Crystals from monohydrated calcium oxalate, uric acid, and triple phosphate are birefringent under polarized microscopy. Urinary crystals can be useful in the diagnosis of urolithiasis. Crystal formation can occur in normal urine when cooled; therefore, only fresh urine samples should be analyzed for crystals.
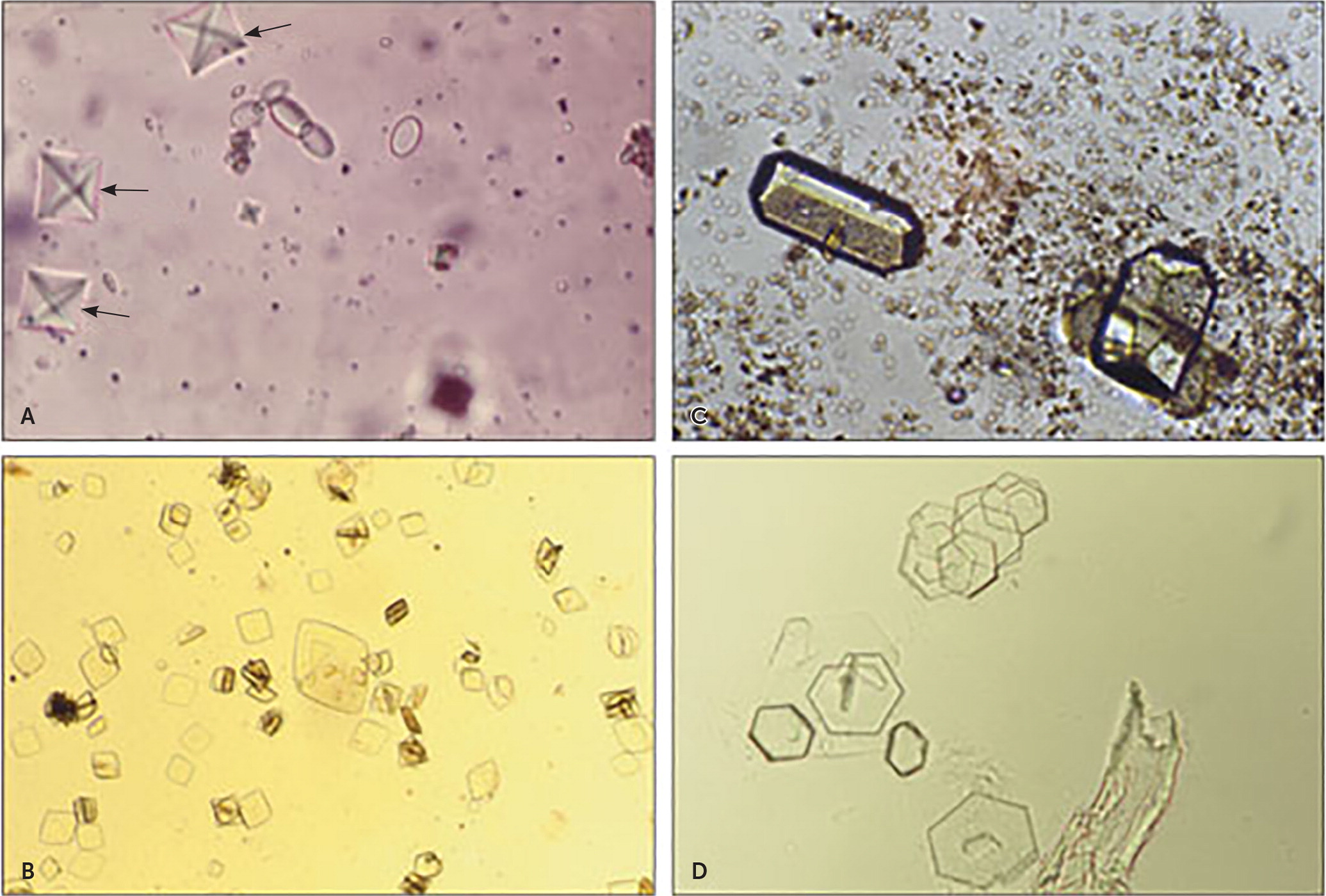
The presence of casts in urine (eFigure B) suggests certain renal pathologies (Table 86). Hyaline casts are made of protein and may be a normal finding or occur with renal disease. RBC and WBC casts confirm glomerular disease. Granular casts consist of protein or degraded cellular casts and may indicate tubular injury, such as acute tubular necrosis.6,25
This article updates previous articles on this topic by Simerville, et al.,6 and Sharp, et al.24
Data Sources: A PubMed search was completed in Clinical Queries using the key terms urinalysis, dipstick, and UTI. Also searched were Essential Evidence Plus, the Cochrane database, and reference lists in retrieved articles. Search dates: January 25, 2021, and January 25, 2022.
