
Am Fam Physician. 2023;107(6):613-622
Patient information: See related handout on benign prostatic hyperplasia.
Author disclosure: No relevant financial relationships.
Lower urinary tract symptoms from benign prostatic hyperplasia affect 25% of U.S. men, nearly one-half of whom have at least moderate symptoms. Sedentary lifestyle, hypertension, and diabetes mellitus increase risk of symptoms. Evaluation is focused on determining severity of symptoms and therapy to improve symptoms. Rectal examination has limited accuracy in evaluating prostate size. Transrectal ultrasonography is preferred to verify size when starting 5-alpha reductase therapy or considering surgery. Serum prostate-specific antigen testing is not recommended in routine evaluation of lower urinary tract symptoms, and shared decision-making should be used for cancer screening decisions. The International Prostate Symptom Score is the best way to track symptoms. Self-management methods, including limiting evening fluid intake, reducing caffeine and alcohol intake, toilet and bladder training, pelvic floor exercises, and mindfulness techniques, can improve symptoms. Although saw palmetto is not effective, the herbal treatments Pygeum africanum and beta-sitosterol may be effective. Primary medical treatment involves alpha blockers or phosphodiesterase-5 inhibitors. Alpha blockers offer rapid benefit and can be used for acute urinary retention. Combining alpha blockers and phosphodiesterase-5 inhibitors is not beneficial. For uncontrolled symptoms, 5-alpha reductase inhibitors should be started if the prostate volume is 30 mL or greater by ultrasonography. 5-Alpha reductase inhibitors take up to one year to be fully beneficial and are more effective when taken with alpha blockers. Only 1% of patients with lower urinary tract symptoms require surgery. Although transurethral resection of the prostate improves symptoms, many less invasive options with varying effectiveness can be considered.
Benign prostatic hyperplasia (BPH) is the most common cause of lower urinary tract symptoms in men. This article provides a review of the available patient-oriented evidence to evaluate and manage lower urinary tract symptoms from BPH. Use of the term “men” in this article is intended to include those who have male sex assigned at birth.
| Recommendation | Sponsoring organization |
|---|---|
| Do not order creatinine or upper tract imaging for patients with benign prostatic hyperplasia. | American Urological Association |
Epidemiology
| Risk factor | Explanation |
|---|---|
| Age | Lower urinary tract symptoms generally occur in men older than 30 years and become more prevalent with age. |
| Alcohol | Regular, light drinking is associated with increased lower urinary tract symptoms, possibly because of the diuretic effect of alcohol. The effect of moderate to heavy drinking on lower urinary tract symptoms is uncertain. |
| Cigarette smoking | Severe symptoms are associated with a smoking history of 50 pack-years or more. The effect of lower levels of smoking is unclear. |
| Diabetes mellitus | Increasing insulin is associated with increased prostate volume and symptoms in men older than 60 years. |
| Hypertension | Hypertension is associated with more lower urinary tract symptoms and larger prostate volumes and may decrease the effectiveness of treatment with alpha blockers. |
| Obesity | Lower urinary tract symptoms become more prevalent as body mass index increases; there is some evidence of increasing incidence of lower urinary tract symptoms in men who are obese and younger than 30 years. |
| Sedentary lifestyle | Lack of daily walking is associated with progression in lower urinary tract symptoms, and lower urinary tract symptoms are more prevalent in men who exercise less. |
Diagnosis
Potential causes of lower urinary tract symptoms are identified with patient factors.5 Relevant history includes fluid intake; history of sleep apnea; having diabetes mellitus, heart failure, hypertension, chronic kidney disease, or neurologic disorders; family cancer history; and tobacco use, alcohol consumption, sexual history, and current medications.
Important family history can include urethral, bladder, prostatic, or urothelial cancer. Having multiple sex partners increases risk of prostatitis.
The differential diagnosis for lower urinary tract symptoms is summarized in Table 2.6,7 Overactive bladder syndrome and detrusor overactivity are common and can exacerbate BPH.
| Anatomic Foreign body Urethral or bladder neck strictures Infections Prostatitis Urethritis or sexually transmitted infections Urinary tract infection Inflammatory conditions Chronic pelvic pain syndrome or chronic prostatitis Malignancy Bladder cancer Prostate cancer | Medications Anticholinergics (e.g., tolterodine) Antihistamines (e.g., diphenhydramine) Bronchodilators (e.g., albuterol) Diuretics Opioid analgesics Sympathomimetics (e.g., pseudoephedrine) Tricyclic antidepressants (e.g., amitriptyline) Neurologic conditions Neurogenic bladder Overactive bladder (detrusor overactivity): can be neurologic, but most cases are idiopathic |
SIGNS AND SYMPTOMS
BPH should be considered in men with voiding difficulties or urinary incontinence.
Voiding symptoms include urinary hesitancy, delay in initiating, intermittency, weak urinary stream, and dysuria.2,8
Storage symptoms include urinary frequency, nocturia, urgency, enuresis, and incontinence.2,8
Post-urination symptoms include sensation of incomplete voiding and urine dribbling.2,8
The American Urological Association recommends the International Prostate Symptom Score (IPSS),5 shown in Table 3, which was originally called the American Urological Association symptom index9,10; it is the only symptom score to significantly predict urinary retention. An IPSS of 20 or higher, demonstrating severe lower urinary tract symptoms, has a positive likelihood ratio of 1.5 for bladder outlet obstruction; an IPSS of less than 20 has a negative likelihood ratio of 0.8.10
Many neurologic conditions can cause or worsen lower urinary tract symptoms.
| Question | 0 Points | 1 Point | 2 Points | 3 Points | 4 Points | 5 Points |
|---|---|---|---|---|---|---|
| Not at all | Less than one time in five | Less than half the time | About half the time | More than half the time | Almost always | |
| During the past month or so, how often have you had a sensation of not emptying your bladder completely after you finished urinating? | □ | □ | □ | □ | □ | □ |
| During the past month or so, how often have you had to urinate again less than two hours after you finished urinating? | □ | □ | □ | □ | □ | □ |
| During the past month or so, how often have you found you stopped and started again several times when you urinated? | □ | □ | □ | □ | □ | □ |
| During the past month or so, how often have you found it difficult to postpone urination? | □ | □ | □ | □ | □ | □ |
| During the past month or so, how often have you had a weak urinary stream? | □ | □ | □ | □ | □ | □ |
| During the past month or so, how often have you had to push or strain to begin urination? | □ | □ | □ | □ | □ | □ |
| None | One time | Two times | Three times | Four times | Five or more times | |
| During the past month, how many times did you most typically get up to urinate from the time you went to bed at night until the time you got up in the morning? | □ | □ | □ | □ | □ | □ |
PHYSICAL EXAMINATION
Physical examination focuses on suprapubic and genital regions to exclude other causes of lower urinary tract symptoms.7
Cardiac examination can reveal hypotension or lower extremity edema.
Abdominal examination can reveal bladder enlargement.
Neurologic examination can reveal sensory deficits.
Genital examination can identify urethral discharge, phimosis, penile lesions, or meatal stricture.
Digital rectal examination can evaluate for prostate size, consistency, and tenderness; however, the examination reliably identifies only prostates larger than 50 mL.7
DIAGNOSTIC TESTING
Urinalysis should be ordered to look for glucosuria, proteinuria, hematuria, and evidence of infection, with urine culture if necessary.2
Prostate-specific antigen (PSA) testing is not required for patients with lower urinary tract symptoms. Serum PSA is a limited predictor of prostate volume, risk of acute urinary retention, and need for surgery.11,12 Discussion of the risks and benefits of prostate cancer screening for shared decision-making is recommended before PSA testing for men 55 to 69 years of age; testing is discouraged in men 70 years or older.13
Renal function testing is recommended only if renal insufficiency is a concern.
Urologists sometimes perform postvoid residual testing, uroflowmetry, and transrectal ultrasonography. However, postvoid residual testing is not useful for routine testing, with a positive predictive value of 63% and negative predictive value of 52% for bladder outlet obstruction.5 Uroflowmetry is not useful for initial evaluation of lower urinary tract symptoms.5
Transrectal ultrasonography is more accurate than digital rectal examination at measuring prostate size. The American Urological Association recommends transrectal ultrasonography before treatment with 5-alpha reductase inhibitors or surgery.5 However, the evidence that prostate-size measurement before medication initiation improves outcomes is limited.
Treatment
The goal of treatment for BPH is to reduce lower urinary tract symptoms, prevent disease progression, and prevent complications such as urinary retention.
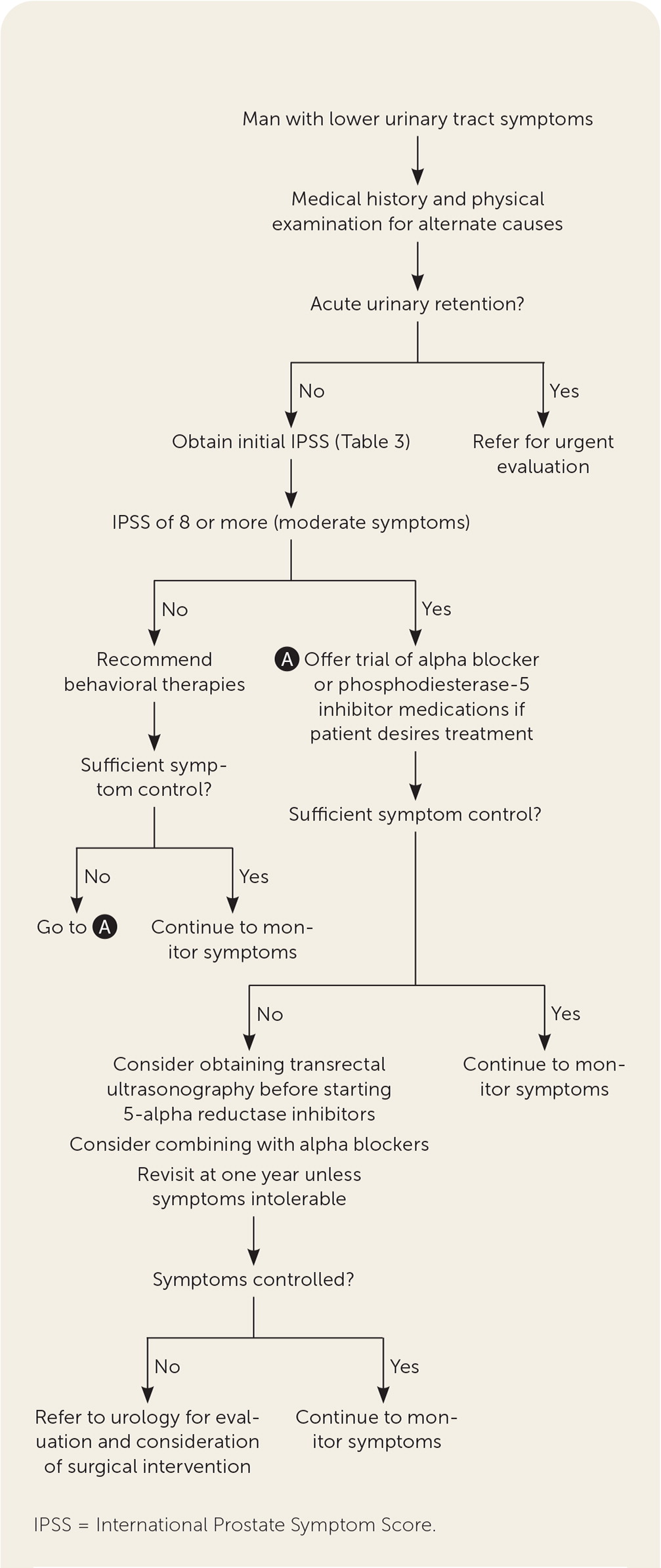
Figure 1 shows a suggested approach to treatment of BPH.
LIFESTYLE INTERVENTIONS
Low- to moderate-quality evidence suggests improvement in symptoms with self-management techniques, such as limited evening fluid intake, reduction of caffeine and alcohol intake, and toilet and bladder training. Toilet training involves techniques, such as double voiding, a repeated urination effort and urethral milking, and massaging the urethra from behind the scrotum toward the base of the penis. Bladder training involves incremental delayed voiding to regain bladder control as well as pelvic floor exercises or mindfulness.5,14–16
Low-quality evidence suggests that sitting while urinating reduces postvoid urinary volume.17
MEDICAL THERAPY
Table 4 provides first- and second-line medication treatment options for lower urinary tract symptoms of benign prostatic hyperplasia.5,8,11,12,18–24
Alpha-blockers and phosphodiesterase-5 inhibitors are first-line therapies. Combining these medications increases adverse effects, such as headache and muscle pain, with only slightly added benefit.8,19
Use of alpha-blockers leads to rapid improvement in lower urinary tract symptoms compared with placebo, based on 19 randomized controlled trials with nearly 10,000 participants.11 Symptom improvement is consistent among different alpha blockers.18
The nonselective alpha blockers terazosin and doxazosin (Cardura) lower blood pressure more than the selective alpha-1 blockers tamsulosin (Flomax) and alfuzosin (Uroxatral).25
Selective alpha blockers are more likely to cause ejaculatory dysfunction,8 whereas nonselective alpha blockers are more likely to cause orthostatic hypotension.18 A small trial suggests that taking selective alpha blockers every other day improves ejaculatory dysfunction while maintaining benefit.26
If cataract surgery is being considered, avoid alpha blockers until ophthalmologist evaluation because of associated floppy iris syndrome.25
For patients with acute urinary retention, immediately start an alpha blocker at urinary catheterization and treat the patient for three days before attempting to remove the catheter.5
Phosphodiesterase-5 inhibitors, such as tadalafil (Cialis), are similarly effective when used as alpha blockers, even in patients without erectile dysfunction, based on a Cochrane review of four randomized controlled trials with 933 participants.8 Phosphodiesterase-5 inhibitors should be a first-line option in men with coexisting BPH and erectile dysfunction.
5-Alpha reductase inhibitors, such as finasteride and dutasteride, improve lower urinary tract symptoms, especially in men with low urinary flow or large prostates on ultrasonography, based on several long-term randomized controlled trials, including more than 1,000 patients.5
The American Urological Association recommends 5-alpha reductase inhibitors if prostate volume is 30 mL or greater on imaging, the prostate is enlarged on examination, or PSA levels exceed 1.5 ng per mL (1.5 μg per L).5 Although the guideline states that a minimum prostate size of 30 mL is required for effective response from a 5-alpha reductase inhibitor, the evidence referenced notes that men with small prostates tend to respond to placebo, whereas those with larger prostates do not. 5-Alpha reductase inhibitors can improve symptoms in all men, although slightly less so in those with smaller prostates.
5-Alpha reductase inhibitors have delayed effect, and the full effect can take up to one year. Benefits of 5-alpha reductase inhibitors last up to 10 years.20,21
Finasteride decreases the progression of BPH at four years with a number needed to treat of 20 (95% CI, 13 to 50) compared with placebo. Finasteride also appears to decrease the risk of urinary retention and surgical intervention.20
Finasteride does not reduce progression of lower urinary tract symptoms compared with doxazosin, but combining finasteride and doxazosin decreases symptom progression.20
Dutasteride improves symptoms and decreases the risk of future urinary retention and surgery.21
Combining 5-alpha reductase inhibitors and alpha blockers is more effective than either medication alone after more than one year. However, at one year or less, no difference occurs.12
The primary adverse events associated with 5-alpha reductase inhibitors are erectile dysfunction, decreased libido, and abnormal ejaculation, with each having one more occurrence per 100 person-years with finasteride than placebo.20,21
5-Alpha reductase inhibitors decrease PSA values by up to 50%, so the physician should consider doubling PSA values for cancer screening interpretation. Men taking 5-alpha reductase inhibitors have delayed diagnosis of prostate cancer, slightly higher risk of high-grade cancers, and worse cancer outcomes.5,22
Anticholinergic medications, which include solifenacin (Vesicare), oxybutynin, and tolterodine, can be used alone or in combination with alpha blockers in patients with lower urinary tract symptoms that are primarily storage symptoms, although the evidence of benefit is uncertain.23 Use of these medications is limited by risks of acute urinary retention, dementia, and mental status changes, especially in older men.24
Beta-3 agonist mirabegron (Myrbetriq) does not improve lower urinary tract symptoms more effectively than placebo.27
Desmopressin appears to minimally improve nocturia compared with placebo.28
| Medication class | Evidence summary | Pros | Cons |
|---|---|---|---|
| First line | |||
| Alpha blockers | Lower IPSS by 2 to 4 points based on 21 RCTs with more than 10,000 patients11 | Improvement is a class effect Rapid improvement of symptoms Low cost | Caution with use around cataract surgery because of floppy iris syndrome Adverse effects of orthostatic hypotension and ejaculatory dysfunction8,18 |
| Phosphodiesterase-5 inhibitors | Demonstrate similar effectiveness to alpha blockers based on a Cochrane review of four trials with 933 patients8; effect is the same in patients without erectile dysfunction | Dual effects in patients with both BPH and erectile dysfunction | Combination with alpha blockers has only slight added benefit over either medication alone Mild adverse effect of headache is most common11,19 |
| Second line | |||
| 5-Alpha reductase inhibitors | Lower IPSS score by 1 to 2 points based on 14 RCTs with nearly 15,000 patients11 Decreased volume of prostate by 15% to 25% at six months based on three RCTs with nearly 4,000 men5 | Decrease progression of BPH at four years Decrease the risk of urinary retention and surgical intervention20 Combining with alpha blockers is more effective than either medication alone at one year12 | Full symptom improvement can take up to a year Adverse effects of erectile dysfunction, decreased libido, and abnormal ejaculation20,21 Decreases prostate-specific antigen value; risk of delay in diagnosis of prostate cancer 22 |
| Anticholinergics | Combination therapy with alpha blockers lowers IPSS score by 2 points compared with alpha blockers alone; evidence from 19 RCTs with 3,631 patients, but very low certainty because of high risk of bias and heterogeneity 23 | Combining with alpha blockers may improve quality of life but is uncertain in clinical significance23 | Risks of acute urinary retention, dementia, and mental status changes, especially in older population24 |
COMPLEMENTARY THERAPY
Use of saw palmetto does not improve lower urinary tract symptoms or prostate volume compared with placebo, based on high-quality evidence from 32 long-term randomized controlled trials of 5,666 men.29
Small, short-duration, low-quality studies suggest improvement in lower urinary tract symptoms and urinary-flow measurement with Pygeum africanum.30
Beta-sitosterol, a phytotherapeutic compound, appears to improve urinary symptoms and flow measures; however, its long-term effectiveness and safety are unknown.31
In one small, low-quality study, acupuncture did not improve lower urinary tract symptoms.32
SURGICAL THERAPY
Indications for surgical intervention may include failure of lifestyle interventions and medical therapy, a desire to avoid daily medications, intolerable adverse effects, or signs of poor control such as renal insufficiency, urinary retention, recurrent urinary tract infections, or recalcitrant gross hematuria.33
Of men who are treated for lower urinary tract symptoms from BPH, 1% have a procedural or surgical intervention.2
Decisions about specific surgical or minimally invasive surgical therapies should involve shared decision-making regarding procedural risks, which likely include sexual adverse effects, procedure effectiveness, and retreatment risk.33
Table 5 lists surgical options for BPH.33–49 Transurethral resection of the prostate (TURP) is the primary treatment for lower urinary tract symptoms from BPH that is uncontrolled despite medical therapy for average-sized prostates (30 mL to 80 mL). TURP is the most effective treatment option. Risks include bleeding, incontinence, and adverse sexual effects.34
Several minimally invasive surgical therapies have fewer adverse effects than TURP, but many lack high-quality data or have higher retreatment rates. However, many minimally invasive surgical therapies are office-based procedures that do not require general anesthesia or anticoagulation discontinuation.
For small-sized prostates (less than 30 mL), TURP or the minimally invasive transurethral incision of the prostate should be considered.50
For large-sized prostates (more than 80 mL), simple prostatectomy is recommended over TURP. Bipolar transurethral enucleation of the prostate or holmium laser enucleation of the prostate are less invasive alternatives to prostatectomy.51
| Procedure | Description | Evidence summary | Pros | Cons |
|---|---|---|---|---|
| TURP | Prostate tissue is surgically removed via a urethrally placed resectoscope | Based on meta-analysis of 20 RCTs with up to five years of follow-up: 70% reduction in symptoms by IPSS, 69% improvement in quality of life34 | Robust data with proven long-term outcomes Bipolar TURP reduces risk of hyponatremia and transurethral resection syndrome | Inpatient procedure Longer hospital stay Risk of complications, such as erectile dysfunction, irritative voiding, bladder neck contracture, blood transfusion, urinary tract infection, or hematuria Risk of transurethral resection syndrome (monopolar) Difficult to remove enough tissue for very large prostates |
| Simple prostatectomy | Removal of prostatic obstruction using an open, laparoscopic, or robotic method | Small RCT compared simple prostatectomy with TURP in patients with prostate volume > 80 mL and found that prostatectomy was no slower, was more effective, and may be safer in this population35 | Can be performed on large (> 80 mL) prostates when the size cannot be addressed by a transurethral approach Removes more prostatic tissue than TURP | Most invasive treatment option Open prostatectomy has increased risk of bleeding and transfusions Robotic prostatectomy has increased operative times and steeper learning curve Rates of complications are similar to TURP |
| Transurethral incision of the prostate | Incision of the bladder outlet without removing prostatic tissue | Systematic review of nine RCTs comparing TURP vs. transurethral incision of the prostate in patients with mean prostate size < 30 mL found similar symptom improvement at 12 months, with fewer complications in the transurethral incision of the prostate group36 | Outpatient procedure Less blood loss and shorter stay than with TURP Reduced ejaculatory problems Can be performed if the prostate is small (< 30 mL) | Higher rate of repeat procedure compared with TURP Lack of large, high-quality studies with long-term outcomes |
| Bipolar transurethral enucleation of the prostate | Uses bipolar high-frequency generator to surgically remove prostatic obstruction | In a small RCT of 240 patients with prostates > 80 mL, patients with bipolar transurethral enucleation of the prostate had less anemia and more symptom improvement at 24 months compared with TURP37 | Similar symptom and quality of life improvement compared with TURP Removes more prostate tissue, has less blood loss, and shorter indwelling catheter time Can treat large prostates | Longer operative time than TURP Limited long-term evidence |
| Holmium laser enucleation of the prostate | Use of holmium laser for tissue coagulation and necrosis that allows removal of large volume of prostate | Systematic review of 12 trials found that holmium laser enucleation of the prostate slightly improves symptoms by IPSS (−1.17; 95% CI, −0.41 to −1.93), shortens hospital stay (mean difference, −24.3 hours; 95% CI, −35.8 to −12.9) with similar quality of life and complication rates38 | Lower risk of transurethral resection syndrome Shorter catheterization time and length of hospital stay Fewer blood transfusions Can be performed for large prostates | Inpatient procedure Dependent on surgeon's level of expertise Higher risk of dysuria, retention, and repeat procedure compared with TURP Lack of large, high-quality studies with long-term outcomes |
| Laser photo vaporization of the prostate | Green light laser that is absorbed by hemoglobin but not water, allowing vaporization and removal of prostatic tissue with adequate hemostasis | Systematic review of 45 RCTs comparing laser photo vaporization of the prostate to TURP found no significant difference in symptoms; laser photo vaporization of the prostate leads to fewer transfusions and shorter hospital stays39 | Outpatient procedure Patients can remain on anticoagulation Less bleeding compared with TURP Similar IPSS scores compared with TURP | Slower and less prostatic tissue removed than with TURP Lack of large, high-quality studies with long-term outcomes |
| Prostatic urethral lift | Cystoscopic-guided placement of small permanent sutures that compress encroaching lateral lobes opening the prostatic urethra | Small, unblinded RCT of 91 patients comparing prostatic urethral lift with TURP found more preservation of ejaculatory function with prostatic urethral lift (100% vs. 61%; P < .0001) but less improvement in lower urinary tract symptoms40 | Can be performed with local anesthesia Preservation of erectile and ejaculatory function | Must have an absence of a middle prostatic lobe |
| Transurethral microwave therapy | Delivery of energy through transurethral microwave antenna to produce coagulation necrosis of prostatic tissue | Cochrane systematic review of six RCTs comparing transurethral microwave therapy with TURP found similar reduction in urinary symptoms, with transurethral microwave therapy having fewer major adverse effects (number needed to treat = 8; 95% CI, 7 to 11) but with a higher risk of retreatment in one year (number needed to harm = 12; 95% CI, 7 to 25; relative risk = 0.2; CI, 0.09 to 0.43)41 | Outpatient procedure Lower risk of erectile and ejaculatory dysfunction, strictures, incontinence, and blood transfusions compared with TURP | High retreatment rate compared with TURP (relative risk = 7.07; 95% CI, 1.94 to 25.82). Increased risk of acute urinary retention (relative risk = 2.61; 95% CI, 1.05 to 6.47) |
| Transurethral prostate convective water vapor thermal therapy | Uses radio-frequency to create steam that delivers thermal energy, causing necrosis of prostatic tissue | RCT with 197 patients comparing water vapor thermal therapy with control therapy found a mean reduction in IPSS of 11.2 points compared with 4.3 points (P < .0001)42 | Preservation of erectile and ejaculatory function IPSSs remain improved up to 36 months | No direct high-quality comparative studies between water vapor thermal therapy and TURP Possible higher retreatment rate |
| Robotic water-jet ablation | Transrectal ultrasound-guided ablation of prostatic tissue using targeted high-velocity saline stream followed by electrocautery hemostasis | RCT of 184 patients randomized to water-jet ablation vs. TURP found similar improvements in IPSS Cumulative adverse events at three months occurred in 25.9% of water-jet ablation group vs. 41.5% of TURP group (P < .02)43 | Shorter resection time compared with TURP Reduced incontinence, erectile dysfunction, and ejaculatory dysfunction | Limited evidence on its effectiveness and longer-term retreatment rates Requires general anesthesia |
| Transurethral needle ablation | Use of a special catheter that incorporates needles to deliver low-level radio-frequency power to a localized area of the prostate | Systematic review of four RCTs comparing transurethral needle ablation with TURP (450 patients) found less improvement in IPSS score (mean difference = 3.9; 95% CI, 1.27 to 6.63) compared with TURP44 | Reduced risk of blood transfusions, strictures, and incontinence compared with TURP | Not currently recommended because of worse symptom outcomes compared with other available procedures |
| Prostatic arterial embolization | Selective embolization of prostatic arterial supply | Cochrane review of six RCTs and two observational studies comparing prostatic arterial embolization with TURP found an unclear difference in IPSS, quality of life, or major adverse events45 | May decrease time with indwelling urinary catheter, hospital stay | Not supported in routine treatment outside of a clinical trial based on the American Urological Association expert opinion because of the referenced Cochrane review reporting low or very low certainty of evidence for these main outcomes |
Prognosis
The American Urological Association recommends using the IPSS to follow improvement and progression.5
Despite lower urinary tract symptoms from BPH affecting approximately two of every three men 50 years or older, only one-third of affected men seek treatment, and only a small number require procedural interventions.2
BPH is associated with a four times higher prostate cancer risk and three times higher bladder cancer risk.46 Prostate cancer screening guidelines are not affected by the presence of BPH.47,48
Editor's Note: Dr. Arnold is a contributing editor for AFP.
This article updates previous articles on this topic by Pearson and Williams52; Edwards53; and Dull, et al.54
Data Sources: PubMed searches were completed using the key terms benign prostatic hyperplasia, benign prostatic hypertrophy, prostatic hyperplasia, prostatic hypertrophy. After the major themes were identified, searches were performed within aspects such as epidemiology, treatment, and surgery. The searches included systematic reviews, meta-analyses, randomized controlled trials, and review articles. We also searched the Cochrane database and Essential Evidence Plus; in addition, references in these resources were searched. Search dates: May, July, and December 2022; April 2023.
The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the U.S. Department of the Army, U.S. Department of the Navy, U.S. Department of the Air Force, Uniformed Services University of the Health Sciences, U.S. Department of Defense, or the U.S. government.
