
Am Fam Physician. 2023;108(4):417-419
Author disclosure: No relevant financial relationships.
A 74-year-old woman presented with severe fatigue. The patient reported being dizzy for the past day, regardless of activity, and a feeling of impending loss of consciousness. She had a history of hypertension and diabetes mellitus. Her ongoing medications were enalapril, 5 mg per day; atenolol, 25 mg per day; and metformin, 750 mg per day.
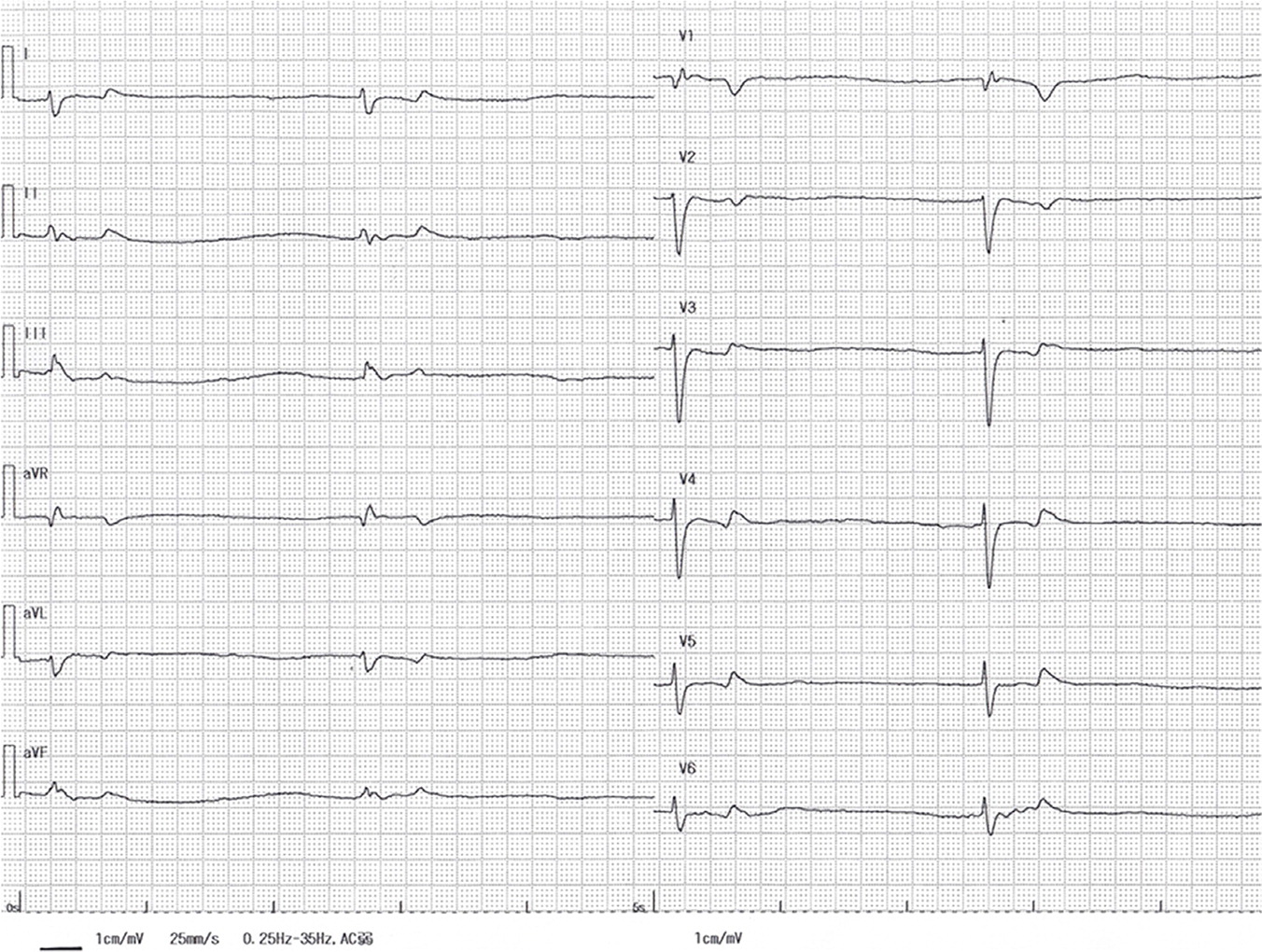
On examination, she had a heart rate of 24 beats per minute, blood pressure of 90/40 mm Hg, respiratory rate of 20 breaths per minute, and peripheral oxygen saturation of 96% on room air. Results of urgent blood testing showed a glucose level of 242 mg per dL (13.43 mmol per L), potassium level of 6.8 mEq per L (6.8 mmol per L), and creatinine level of 3.2 mg per dL (282.88 μmol per L); other values were nearly within the reference range. Twelve-lead electrocardiography was performed (Figure 1).
Question
Based on the patient’s history and physical examination findings, which one of the following is the most likely diagnosis?
A. BRASH syndrome.
B. Long QT syndrome.
C. Myocardial infarction.
D. Sick sinus syndrome.
Discussion
The answer is A: BRASH syndrome. This is a relatively new syndrome, defined as the combination of bradycardia, renal failure, atrioventricular nodal blockade, shock, and hyperkalemia.1 In BRASH syndrome, the synergistic effect of renal failure, hyperkalemia, and medications that block the atrioventricular node leads to progressive bradycardia and hypoperfusion, further aggravating renal failure and hyperkalemia. The result is a cycle of multiorgan failure and potential death.2 Hyperkalemia alone generally requires potassium levels greater than 7 mEq per L (7 mmol per L) to cause bradycardia.3 Bradycardia may occur at lower levels of hyperkalemia due to the synergistic effect of an atrioventricular node blocker. Patients with BRASH syndrome typically do not have enlarged QRS complexes or peaked T waves.
In this patient, the electrocardiogram (ECG) on admission showed a heart rate of 24 beats per minute, junctional rhythm, and a left bundle branch block. A diagnosis of BRASH syndrome was made based on the presence of symptomatic bradycardia with ECG findings, baseline renal dysfunction, hyperkalemia, and long-term treatment with a beta blocker.
According to the advanced cardiac life support algorithm, if the patient shows signs of bradycardia-induced shock, atropine should be administered. If it is ineffective, percutaneous cardiac pacing should be considered.4 Reports of atropine administration and temporar y pacing for BRASH syndrome show limited effectiveness.5 Therefore, using the advanced cardiac life support algorithm may not be effective in patients with BRASH syndrome.
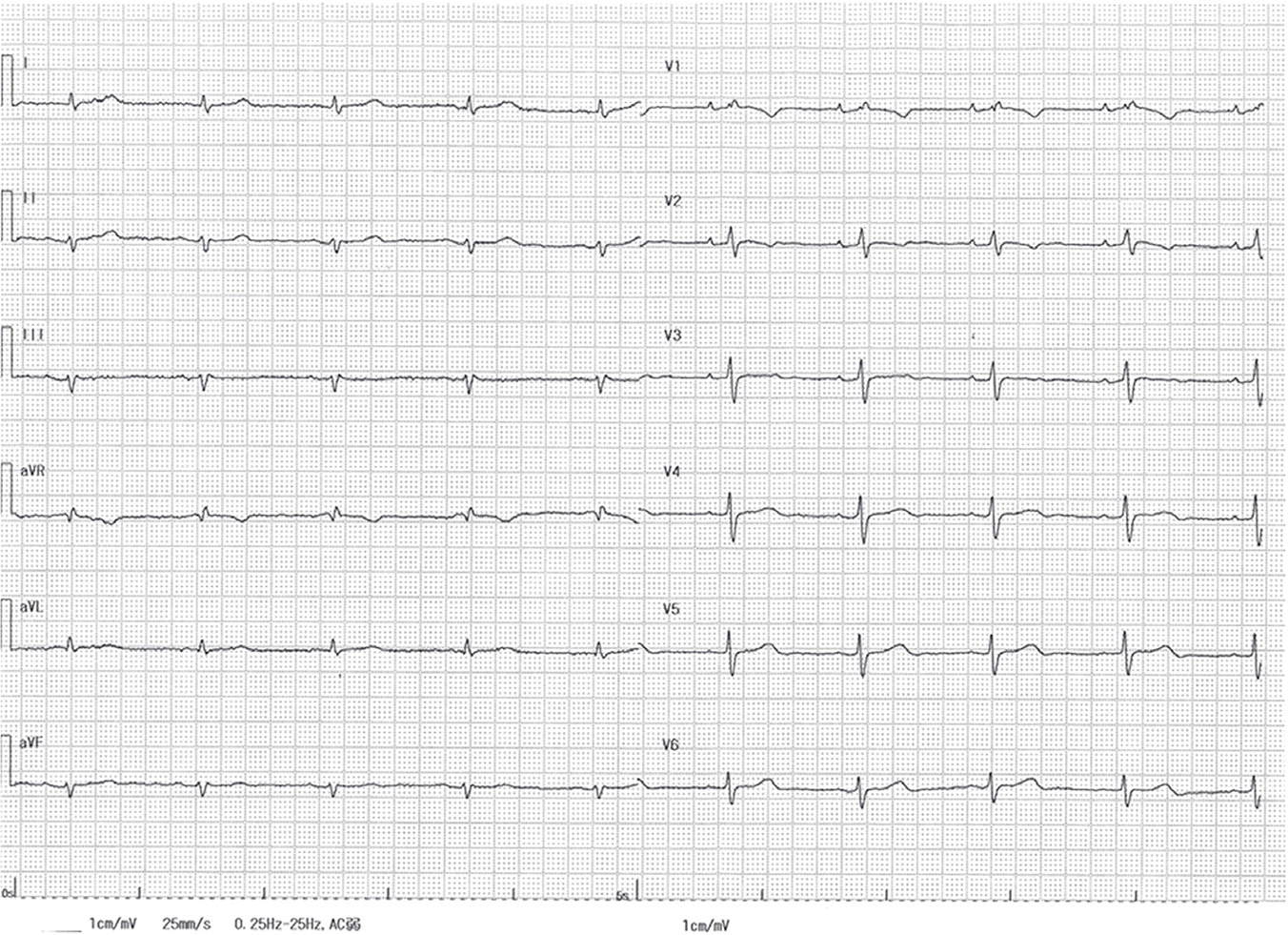
BRASH syndrome is associated with a high rate of dehydration, which necessitates adequate fluid resuscitation. Treatment of BRASH syndrome focuses on rapid management of hyperkalemia with intravenous calcium to stabilize the cardiac membrane.6 In this patient, normal saline and 10 mL of 8.5% calcium gluconate hydrate were infused for rapid fluid resuscitation, and rapid-acting insulin, 0.1 unit per kg per hour, was administered to lower the potassium level. Because her bradycardia was probably caused or precipitated by a beta blocker and her hyperkalemia was caused by an angiotensin-converting enzyme inhibitor, these drugs were discontinued. Within a few hours, her bradycardia improved to 60 beats per minute, her potassium level dropped to 5.8 mEq per L (5.8 mmol per L), and her ECG showed normal sinus rhythm (Figure 2).
Long QT syndrome presents as lightheadedness or presyncope, possibly with palpitations, hypotension, or chest pain. ECG changes include prolonged QTc. The patient may have a history of factors associated with QT prolongation, such as use of certain medications or electrolyte abnormality.
Myocardial infarction of the inferior wall is characterized by ST elevation in ECG leads II, III, and aVF. Reciprocal ST depression may occur in lead aVL.
Sick sinus syndrome is abnormal sinus node function resulting in bradycardia and cardiac insufficiency. The cause may be multifactorial. ECG abnormalities may include sinus bradycardia, sinus arrhythmia, sinoatrial exit block, and sinus arrest.
| Condition | Characteristics |
|---|---|
| BRASH syndrome | Synergistic process from a combination of hyperkalemia and medications blocking the atrioventricularnode; the most common precipitants are use ofhyperkalemic-associated medications and renal injury;an ECG typically shows bradycardia but no findingscharacteristic of hyperkalemia |
| Long QT syndrome | Symptomatic patients present with lightheadedness orpresyncope, possibly with palpitations, hypotension, orchest pain; history of QT-prolonging factors, such asuse of certain medications or electrolyte abnormality;prolonged QTc on ECG |
| Myocardial infarction (inferior wall) | ST elevation in ECG leads II, III, and aVF; reciprocal ST depression may occur in lead aVL |
| Sick sinus syndrome | Abnormal sinus node function resulting in bradycardia and cardiac insufficiency; cause may be multifactorial; ECG abnormalities may include sinus bradycardia, sinus arrhythmia, sinoatrial exit block, and sinus arrest |
