
This is an updated version of the article that appeared in print.
Am Fam Physician. 2023;108(5):519-522
Author disclosures: Dr. Wetterer is in the Physicians for Reproductive Health Leadership Training Academy; Dr. Shenko is a volunteer physician with the Miscarriage and Abortion Hotline; and Dr. Prine is on the leadership team of the Miscarriage and Abortion Hotline and is the executive director of the Abortion Coalition for Telemedicine Access.
Case Scenario
M.A. is a 24-year-old patient who presents to my office two weeks after using abortion pills that she ordered online because abortion is now illegal in this state. M.A. reports that she took 200 mg of mifepristone orally 10 weeks after her last menstrual period. Twenty-four hours later, she took four misoprostol (Cytotec) pills buccally. When nothing happened, she stated that she took another misoprostol dose, after which she experienced heavy bleeding and cramping. Ten days later, she is still bleeding irregularly. She is wondering whether this is normal or whether she is still pregnant. How should I answer her questions? What are my legal risks in this situation?
Commentary
The American politicolegal landscape surrounding abortion and routine pregnancy care has been changing rapidly since the 2022 Supreme Court of the United States issued its decision on Dobbs v. Jackson Women's Health Organization.1
Patients and physicians face uncertainty about how abortion and miscarriage care may be accessed and what legal liability they may face. One grassroots response has included a dramatic increase in accessing medication abortion pills outside established health care systems, such as online pharmacies, telehealth visits with physicians from other countries, or even informal networks.2,3 Patients commonly access resources such as Plan C, Mayday Health, and the Miscarriage + Abortion Hotline (833-246-2632). The hotline is staffed by more than 60 volunteer clinicians—mostly family physicians—and offers medical information via phone and text.2
Family physicians may be asked to evaluate patients who have self-managed an abortion or miscarriage without prior consultation. Studies of medication abortion provision through telemedicine have demonstrated that limited clinical evaluation before using medications for induced abortion is safe and effective; the sparse existing data around self-managed abortion echo these findings.4 Two clinical questions typically arise after self-managed abortion or miscarriage: Is the bleeding normal? and Is the abortion complete?
For the family physician, the medical assessment is identical regardless of whether the bleeding is spontaneous or induced. Treating a resolving miscarriage is the same as treating a self-managed medication abortion. Only clinically relevant information should be documented in the medical record, such as estimated gestational age, timing of bleeding, and any pregnancy symptoms before and after the bleeding.5 The use of pills to start this process does not affect subsequent treatment and may be omitted from the medical record.6
BLEEDING
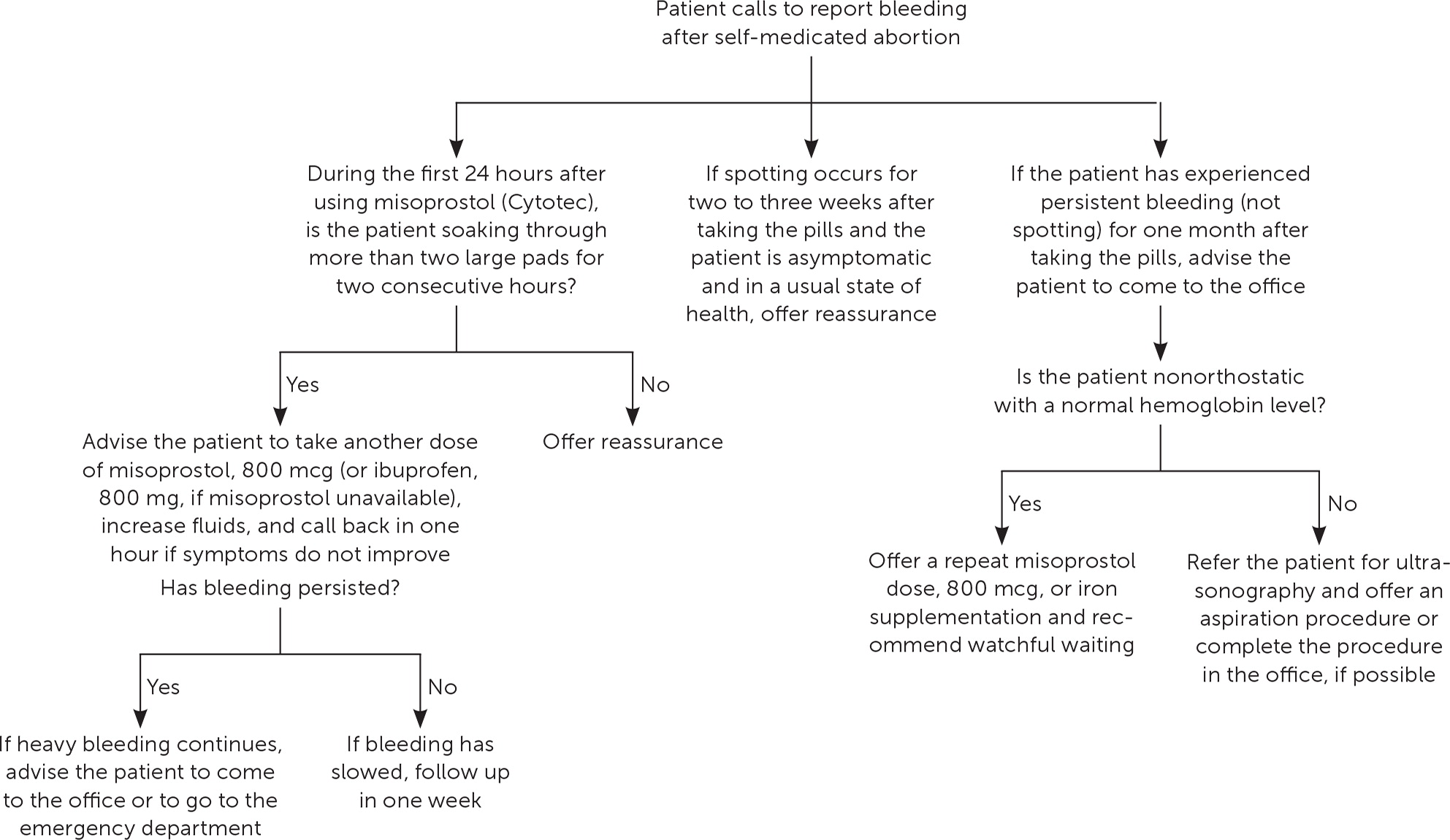
It is rare for miscarriages or abortions to result in life-threatening bleeding.7 Physicians can assess anemia or bleeding as they would for any other medical scenario that might result in symptomatic anemia by asking patients about feeling faint, whether they have maintained hydration during the process, and about the number of pads that they are soaking through. Physicians who evaluate these patients in their office can consider checking a point-of-care hemoglobin level or obtaining a complete blood count. Bleeding is considered worrisome if the patient is soaking through more than two large pads per hour for two consecutive hours (e.g., four large pads in two hours); this occurrence is rare. Figure 1 provides an approach that can help physicians triage phone calls about bleeding.8
ASSESSING FOR COMPLETION
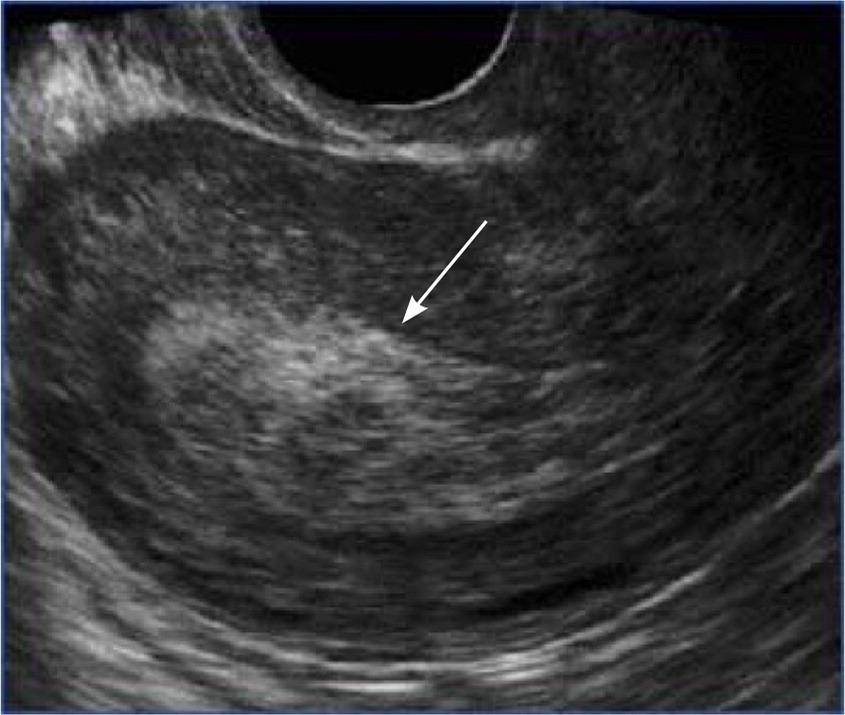
A detailed history of the experience and whether that history correlates with gestational age are important. Bleeding at four weeks' gestational age can be minimal, but at 10 weeks, bleeding is typically quite heavy and may be accompanied by passage of clots and tissue. Importantly, urine and quantitative pregnancy test results are expected to be positive for up to four to six weeks following an abortion or miscarriage. Subjective symptoms and their subsequent resolution (e.g., breast or chest tenderness, nausea, fatigue) are most important for assessing the completion of the abortion or miscarriage.9 Helpful diagnostic testing can include serial quantitative beta human chorionic gonadotropin (beta-hCG) measurement, ultrasonography, or both; this information should be interpreted in the context of the history and gestational age. Ultrasonography that shows thickened endometrium, but no gestational sac, is normal and does not require intervention unless associated with excessive bleeding, fever, or other unusual findings (Figure 210). Although it is reasonable to consider the possibility of ectopic pregnancy, particularly if symptoms include severe unilateral pelvic pain, ectopic pregnancy is rare in the abortion-seeking population without risk factors such as prior ectopic pregnancy, history of tubal surgery, or presence of an intrauterine device.11
Obtaining serial beta-hCG measurements over 48 hours and providing return-to-care precautions are reasonable options. If the risk of ectopic pregnancy is low and the beta-hCG level declines rapidly, the beta-hCG does not need to be trended to zero.
EFFECTIVENESS
Using recommended doses of mifepristone and misoprostol effectively ends a pregnancy 98% of the time; ongoing pregnancy is rare.12 The effectiveness of misoprostol-only regimens is possibly lower, about 85% to 95%, but the most recent research supports that misoprostol-only medication abortions are also up to 99% effective when more doses are used.12 Both regimens are safe, although the misoprostol-only process has more prolonged adverse effects.
If additional intervention is required to help pass retained clots (identified as retained heterogeneous tissue/clot on ultrasonography accompanied by prolonged heavy bleeding and cramping, as defined previously), misoprostol may be prescribed to an outpatient pharmacy. Most patients do not require a procedure to evacuate retained material.
LEGAL CONSIDERATIONS
The Health Insurance Portability and Accountability Act (HIPAA) Privacy Rule protects patient confidentiality regarding abortion, as it does with all forms of health care.13 The rule allows for some disclosures of protected health information when required by law, but this is not mandated.13 In other words, when a law requires such reporting, it is permitted but not required to disclose protected health information. However, to date, no state has passed a law mandating the reporting of patients who have had an abortion in violation of state law, and guidance from the U.S. Department of Health and Human Services clarifies that reproductive health care is not within the HIPAA exception for reporting child abuse.13,14 When state law does not require reporting, sharing protected health information would be a breach of the HIPAA Privacy Rule; law enforcement officials cannot obtain records without a court order. Even with a court order, the law does not require reporting. The HIPAA Privacy Rule applies to all patients regardless of age or immigration status. Physicians should seek legal counsel if they are concerned about their responsibilities under state laws.6,20 [updated]
Family physicians should also be aware of crisis pregnancy centers. These centers, often under the guise of providing pregnancy support services, specifically seek to dissuade patients from accessing full-spectrum reproductive health care, including abortion and contraception.15–17 Patients may be given misleading information about the safety or availability of abortion care, both in general terms or even specifically and erroneously that their pregnancy is past a state's gestational limit for receiving an abortion. Crisis pregnancy centers increasingly offer “abortion reversal,” an unfounded and off-label use of progesterone that the American College of Obstetricians and Gynecologists specifically does not support.18 Of note, many crisis pregnancy centers are not staffed by licensed medical professionals and, therefore, are not mandated to abide by HIPAA or general medical codes of conduct.16
Patients who want more information about their legal rights and risks can call the Repro Legal Helpline (844-868-2812) for more information.19
Case Resolution
At 10 weeks' gestation, as seen with the patient in the case scenario, it is common to need a second dose of misoprostol. The patient may see a grayish clump of tissue pass shortly after the second dose of misoprostol and then expect bleeding to be about as heavy as her period. She should no longer feel nauseated, her breasts should no longer feel tender, and the patient should be reassured that these factors and lack of pregnancy symptoms indicate the pregnancy having passed completely. Light bleeding after an abortion or miscarriage may last for two weeks or longer, and spotting and brownish discharge can continue until the next period. An office pregnancy test is not required in this setting because the result would normally be positive. Ultrasonography may be performed if desired, but follow-up with a home urine pregnancy test four to six weeks after taking the pills is usually sufficient. In the absence of clinically significant bleeding, the patient may be counseled that the tissue typically passes on its own and that the next menstrual cycle may be heavier than their usual menstrual flow. If the patient has persistent pregnancy symptoms one week after using the pills, ultrasonography may be performed; however, true medication abortion failures are uncommon. Failure to pass the pregnancy is typically confirmed on ultrasound imaging that shows continued presence of the gestational sac or fetal pole.
Editor's Note: We strive to provide the best available evidence to safely and respectfully care for patients presenting with undesired pregnancy. We recognize the controversies surrounding this topic, which may require cooperation among health care professionals to optimize care.—Sumi Sexton, MD, Editor-in-Chief
