
Am Fam Physician. 2024;109(2):181-183
Author disclosure: No relevant financial relationships.
A 35-year-old man presented with intermittent shortness of breath and paroxysmal cough that had been present for two weeks. His symptoms were managed conservatively, and he was discharged. Two weeks later, the patient described a burning sensation in his chest that accompanied his coughing episodes. Additionally, his shortness of breath had become persistent, and he reported general deconditioning, such as difficulty in performing his daily aerobic exercise. The patient had borderline hypertension controlled with lifestyle measures, but no other significant medical history. He had never smoked and did not regularly use any medications. The patient did not have a significant family medical history.
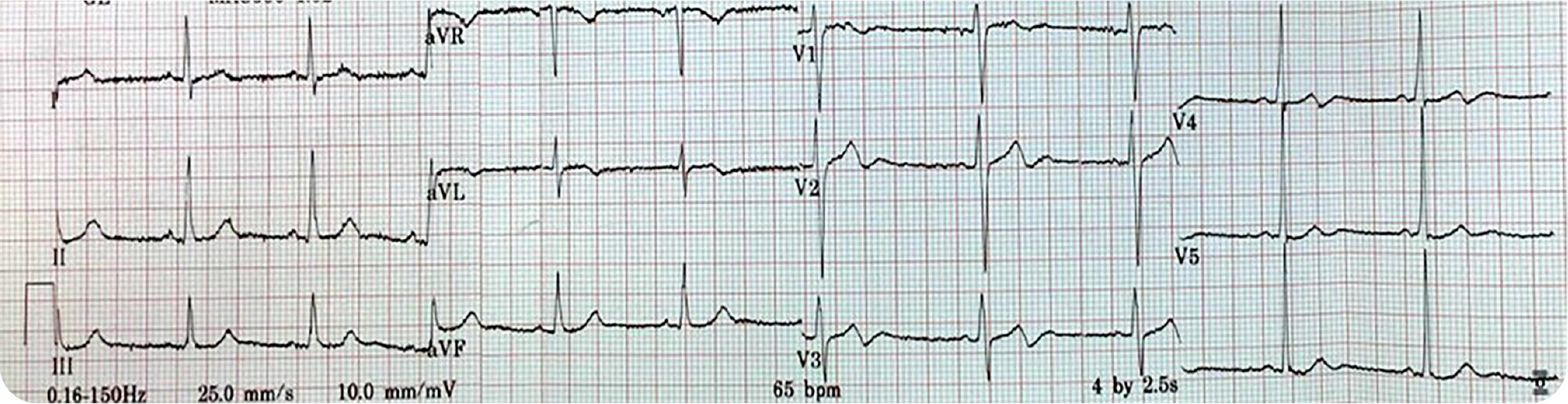
The patient used a clenched fist at the chest (Levine sign)1 to describe his discomfort, but physical examination findings and measurement of vital signs were unremarkable. Due to the patient's use of Levine sign and his history of borderline hypertension, electrocardiography was performed (Figure 1).
Question
Based on the patient's history and physical examination findings, which one of the following is the most likely diagnosis?
A. Brugada syndrome.
B. Hypertrophic cardiomyopathy.
C. Hypokalemia.
D. Pulmonary embolism.
E. Wellens syndrome.
Discussion
The answer is E: Wellens syndrome, defined by deeply inverted or biphasic T waves in leads V2 and V3 that are highly specific for critical stenosis of the left anterior descending coronary artery 2 (Figure 2). This patient had the typical presentation of Wellens syndrome, with episodes of intermittent chest pain caused by sudden occlusion of a previously stenotic coronary artery.3 These episodes are not usually captured by electrocardiography. Reperfusion of the left anterior descending coronary artery by spontaneous clot lysis resolves the chest pain but causes T waves to become biphasic in the corresponding V2 and V3 leads.4
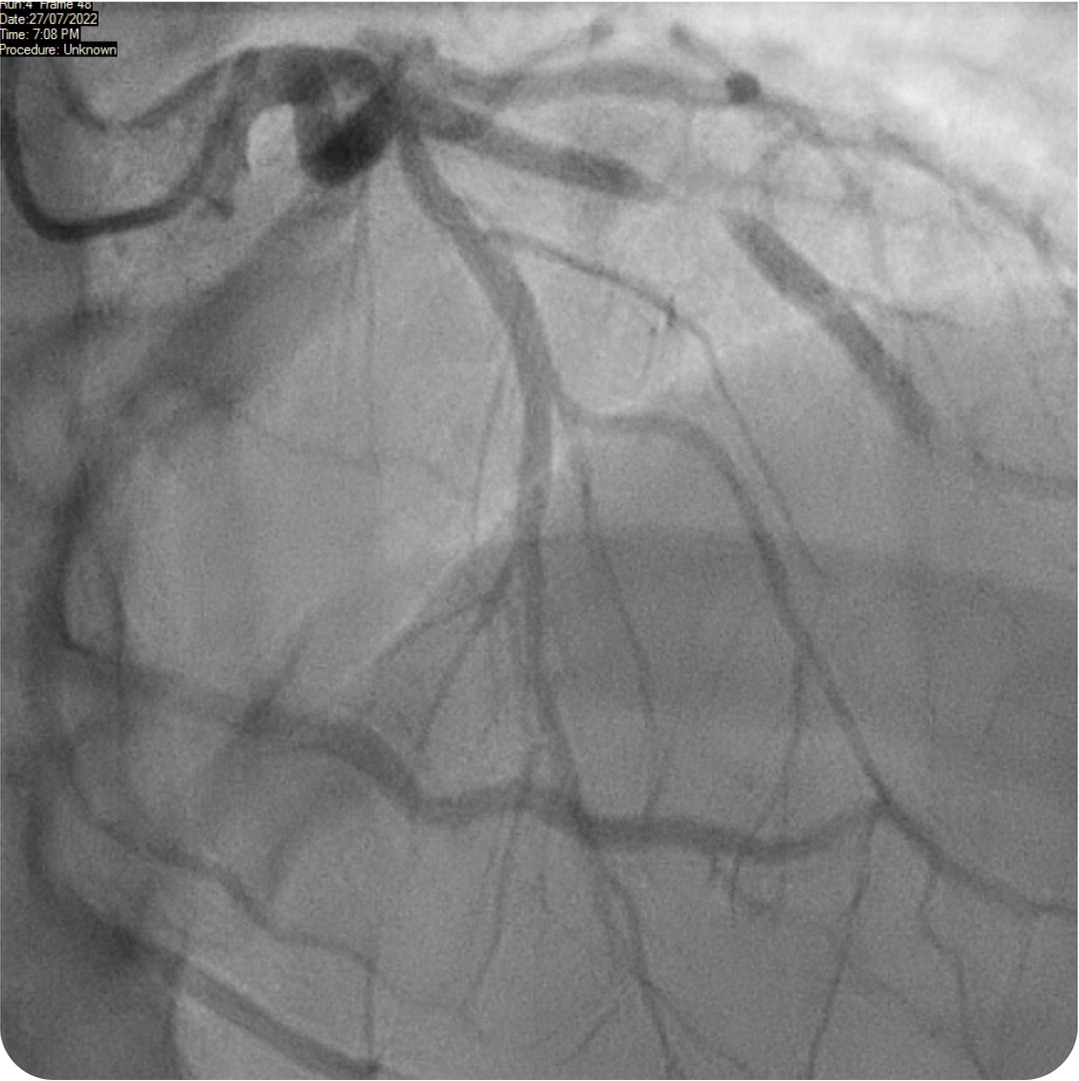
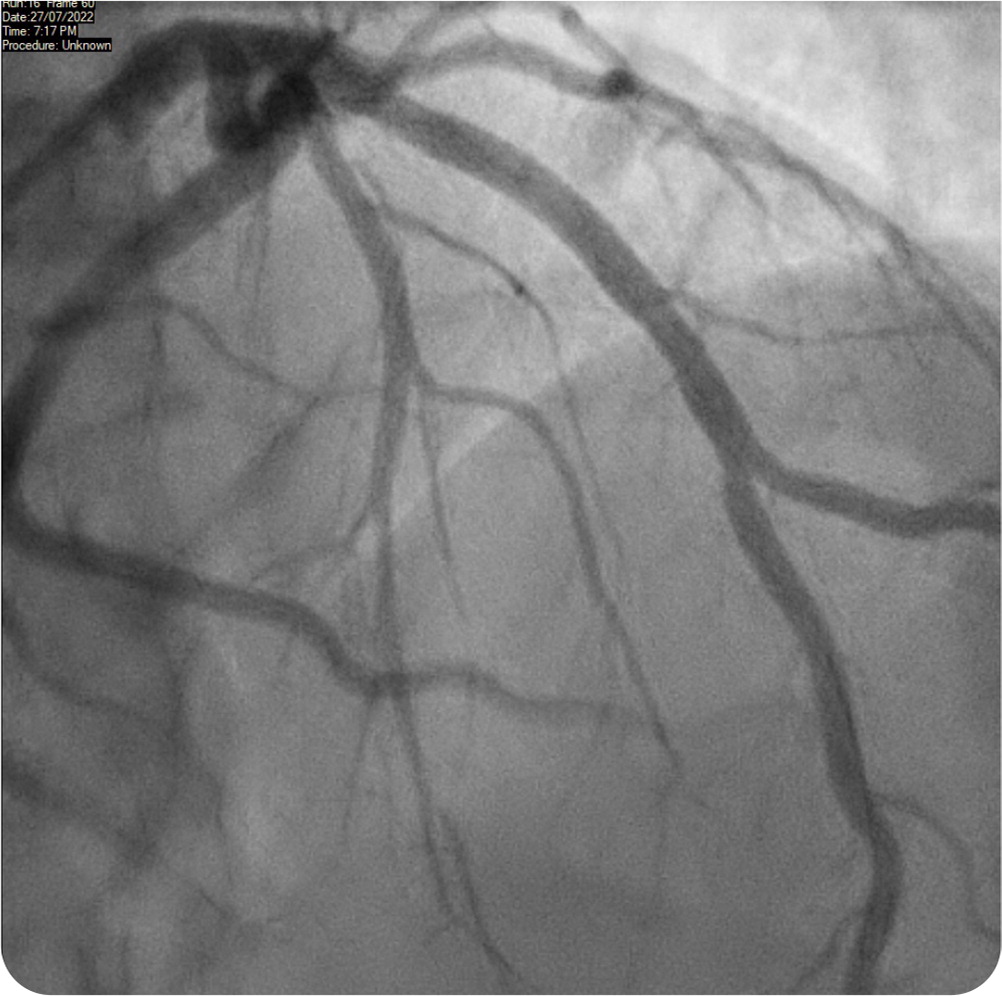
These episodes also feature an isoelectric or minimally elevated ST segment (less than 1 mm), preserved precordial R-wave progression, and a lack of precordial Q waves. Patients have normal or minimally elevated serum troponin levels. This patient was transferred to the emergency department, where repeated electrocardiography showed persistent T-wave changes. Initial troponin levels were normal (34 ng per L [34 mcg per L]), with subsequent measurement showing mild elevation (95 ng per L [95 mcg per L]). Twelve hours later, he underwent percutaneous coronary angioplasty, which revealed 95% stenosis of the proximal left anterior descending coronary artery (Figure 2). The patient was treated with a drug-eluting stent (Figure 3), and subsequent echocardiography showed preserved ejection fraction.
Brugada syndrome can present as T-wave inversions in the right precordial leads (V1 through V3) but also features coved ST-segment elevation, which was not seen in this patient.5,6 Fever and ischemia can induce Brugada syndrome, but this patient had no history of syncope or family history of sudden cardiac death.
Hypertrophic cardiomyopathy is one of the most common inherited cardiac disorders that cause sudden cardiac death among young athletes. It can present as anginal chest pain with exertional dyspnea due to pulmonary congestion. If T-wave abnormalities occur, they are generally deep inversions in the precordial leads. Other common changes indicating left atrial or ventricular enlargement include P mitrale or deep Q waves in the lateral leads.7
Hypokalemia is associated with T-wave changes, generally flattening or inversion. PR prolongation, prominent U waves, and ST depression may also occur.8
Pulmonary embolism typically causes a more pleuritic chest pain. Electrocardiography findings include precordial T-wave inversions (compared with the biphasic T waves seen in Wellens syndrome). Other features include additional T-wave inversions in the inferior leads (right ventricular strain pattern) and the classic finding of sinus tachycardia and incomplete or complete right bundle branch block.
| Condition | Electrocardiography findings |
|---|---|
| Brugada syndrome | T-wave inversions in the right precordial leads (V1 through V3); coved ST-segment elevation |
| Hypertrophic cardiomyopathy | Left atrial enlargement (P mitrale); left ventricular enlargement; deep Q waves in the lateral leads; deep precordial T-wave inversions |
| Hypokalemia | T-wave flattening or inversion; prominent U waves; ST depression; PR prolongation |
| Pulmonary embolism | Sinus tachycardia; T-wave inversions in the precordial or inferior leads (right ventricular strain pattern); incomplete or complete right bundle branch block |
| Wellens syndrome | Deeply inverted or biphasic T waves in leads V2 and V3; isoelectric or minimally elevated ST segment (< 1 mm); preserved precordial R-wave progression; lack of precordial Q waves |
