
Asking patients about their drinking habits is a straightforward way to boost health and revenue.
Fam Pract Manag. 2017;24(3):12-16
The authors wish to acknowledge Joan Newell for her graphics contributions.
Author disclosures: The authors' work was supported by Centers for Disease Control and Prevention cooperative agreement CDC-RFA-DD14-1402, Fetal Alcohol Spectrum Disorders Practice and Implementation Centers. The contents of the article are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention or the U.S. Department of Health & Human Services. No other relevant financial affiliations disclosed.
Excessive alcohol use is far from an isolated problem. Only four percent of the U.S. population meets the diagnostic criteria of having an alcohol use disorder, but almost one in three U.S. adults falls into the “risky” drinking category, and 38 million U.S. adults “binge drink” each year (defined as drinking more than four drinks for women and five drinks for men within a two-hour period).1,2
Most of these drinkers are unaware of the dangers, and many probably consider themselves merely “social” drinkers. However, risky alcohol use can lead to motor vehicle crashes, arrest, intimate partner violence, and medical problems including hypertension, gastritis, liver disease, and cancer.3 Moreover, if a woman drinks while pregnant, the child may be born with a fetal alcohol spectrum disorder, causing lifelong developmental and intellectual disabilities.
As a family physician, you can efficiently and productively address risky drinking with the many patients in your practice who are affected by it. Alcohol screening and brief intervention (aSBI) has been shown to reduce risky drinking and is similar to the blood pressure or tobacco screening you likely already perform in your available for payment. This article describes three steps to seamlessly implement aSBI into your practice:
1) Establish a practice workflow,
2) Incorporate aSBI prompts into your electronic health record (EHR) system,
3) Ensure appropriate coding to receive payment.
VIDEO: BRIEF ALCOHOL INTERVENTION
Alicia Kowalchuk, DO, discusses incorporating alcohol screening into patient visits and demonstrates a brief intervention.
Copyright © 2017 Alicia Kowalchuk, DO
Adding aSBI to the practice workflow
Every practice is unique, so implementing aSBI can be handled in multiple ways. Nevertheless, there are several guiding principles.
First, it is important to identify a practice champion that will promote the use of aSBI within the practice. This person plays a crucial role both as a content resource related to aSBI techniques and as a role model and advocate for maintaining enthusiasm and sustainability within the office. The practice champion will also help identify and overcome any barriers that might get in the way of implementing or sustaining aSBI.
Next, evaluate the current patient flow in the practice. Successful implementations naturally integrate aSBI into practice.1 Moreover, aSBI is considered a grade B recommended service by the American Academy of Family Physicians and the U.S. Preventive Services Task Force and is currently a proposed measure for the 2018 Healthcare Effectiveness Data and Information Set (HEDIS).4,5,6
Using a validated screening instrument such as the National Institute on Alcohol Abuse and Alcoholism Single-Question Test or the U.S. Alcohol Use Disorders Identification Test Consumption (USAUDIT-C) takes only a few minutes for most patients but can help them make healthier choices regarding alcohol use.7,8,9 If a brief intervention is necessary, reimbursement codes are the established workflow, involving multiple professionals in the office rather than depending on the physician alone to incorporate. For example, your office could include a prescreening instrument in the patient intake forms the front desk personnel asks patients to fill out or embed these questions in an existing form that asks about nutrition, exercise, depression, and other health-related behaviors. (See “Alcohol prescreening questionnaire.”) The medical assistant or nurse who rooms the patient could score the questionnaire and determine the need for a full screening instrument, such as the USAUDIT full questionnaire, and administer it when appropriate. That information would be documented in the patient's record for the physician to review. Depending on the result, the physician could engage in a brief intervention to support the patient either cutting back or quitting alcohol use. In practices with integrated behavioral health services, a behaviorist could meet with the patient for a more in-depth discussion or refer the patient to more formal alcohol treatment resources.
Note that most payers require a brief intervention to last at least 15 minutes. The physician must consider his or her rapport with the patient, the patient's clinical needs, and the significance of the patient's alcohol risk to determine whether to devote the full 15 minutes or less time to the intervention.
ALCOHOL PRESCREENING QUESTIONNAIRE
1) Do you sometimes drink beer, wine, or other alcoholic beverages?
[ ] Yes [ ] No
If you answered "Yes," look as this card showing the size of standard drinks:
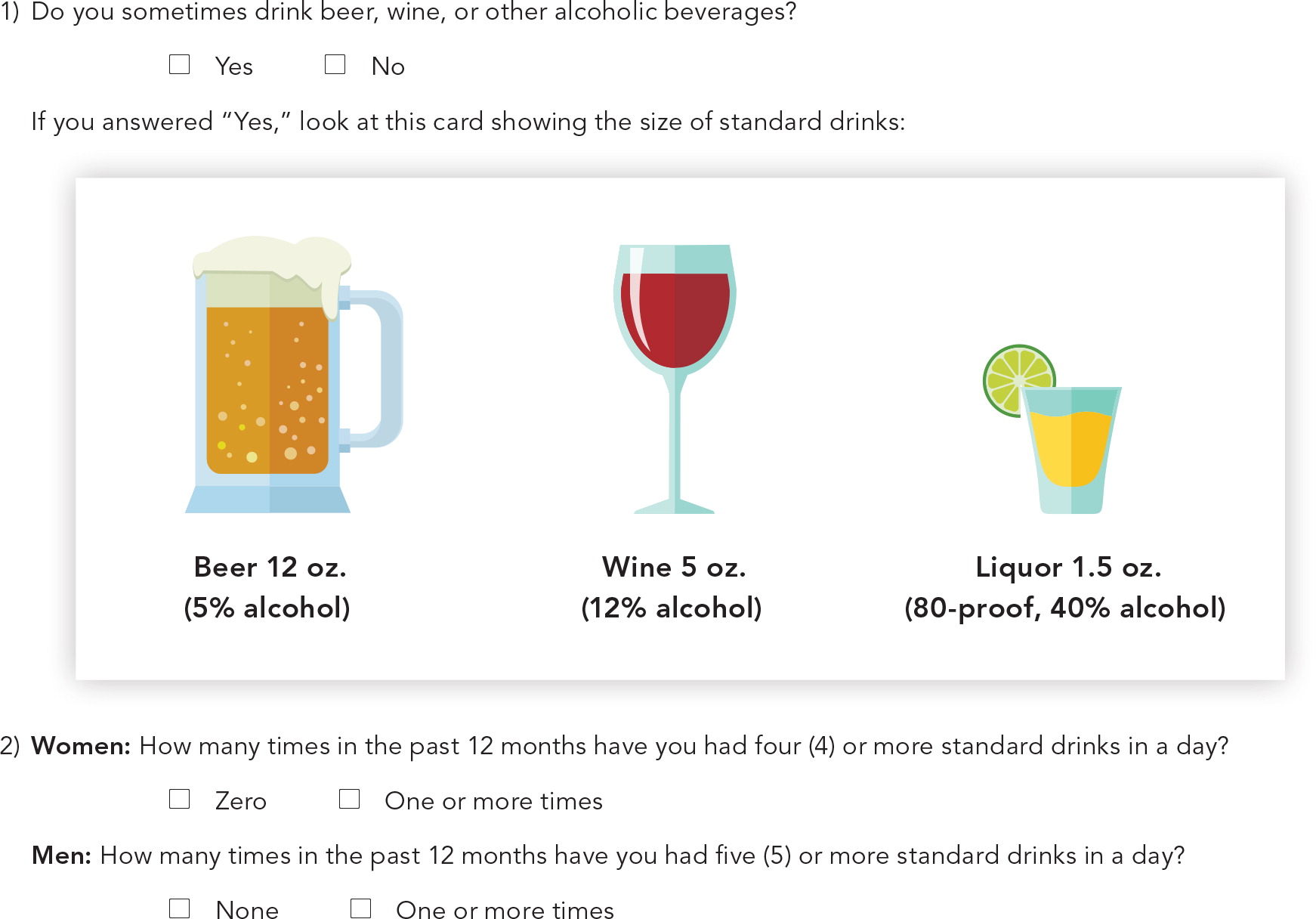
2) Women: How many times in the past 12 months have you had four (4) or more standard drinks in a day?
[ ] Zero [ ] One or more times
Men: How many times in the past 12 months have you had five (5) or more standard drinks in a day?
[ ] Zero [ ] One or more times
Incorporating aSBI prompts into the EHR
The EHR should support aSBI as part of the workflow. Although EHR templates are beyond the scope of this article, the goals should be to capture three key pieces of information: 1) prescreening results, 2) screening scores, and 3) intervention or treatment referral information.10 The EHR needs to be efficient, using searchable data fields and requiring minimal clicks, as that will contribute to long-term sustainability.
Research shows that including alcohol screening reminders in the EHR reinforces the need for screening and prevents the loss of screening documentation.11 Properly designed EHR prompts should guide each professional in the practice through the portion of the screening process relevant for their role. For example, the EHR should prompt the appropriate personnel when an annual prescreening is due and when the results entered warrant a full screen. Embedded prompts can guide the physician through the brief intervention process. Finally, if close follow-up is warranted, the EHR can flag the patient for an appointment in the near future.
Integrating aSBI into the EHR allows the practice to calculate its screening and intervention rates across its patient population for quality reporting purposes and greatly benefits billing and reimbursement for aSBI services.
Getting paid for aSBI
Family physicians will be more enthusiastic about aSBI if they know they will be compensated for their time. Alcohol screening is among the clinical preventive services that the Patient Protection and Affordable Care Act began requiring most insurance plans to cover in 2014, and it is generally covered without patient cost-sharing.12,13 Similarly, annual alcohol screening is covered under Medicare Part B without coinsurance or a deductible.14,15 Furthermore, many states offer some payment for alcohol screening as a preventive service for Medicaid patients, with 16 states doing so without any patient cost-sharing.16
To be paid, the physician or other provider must properly code and bill for the service. A number of CPT codes have been developed for aSBI. Consider the five As model (Ask, Assess, Advise, Assist, and Arrange) when coding and billing. If a patient's initial screening does not warrant a brief intervention, then use Medicare HCPCS code G0442, “Annual alcohol misuse screening, 15 minutes” (asking or assessing under the five As model) or, for commercial insurance, CPT code 96160, “Administration of patient-focused health risk assessment instrument (e.g., health hazard appraisal) with scoring and documentation, per standardized instrument.” However, if a brief intervention is warranted (advising, assisting, or arranging), see the “Alcohol screening and intervention codes” below.
Keep these points in mind to ensure proper coding and payment:
Use a validated screening instrument as recommended earlier in this article. Not doing so may jeopardize payment.
Document both the screening and any necessary intervention.
Document the duration of the intervention. Brief interventions generally must last at least 15 minutes to be reimbursed.
Report CPT codes 99408, 99409, and H0049 with other evaluation and management (E/M) codes by using modifier 25, “Significant, separately identifiable E/M service by the same physician or other qualified health care professional on the same day of the procedure or other service,” or modifier 59, “Distinct procedural service” for non-E/M services.17
Confirm the proper coding and billing approaches with your payers.
| Payer | Code | Description | Fee schedule |
|---|---|---|---|
| Commercial insurance, Medicaid | 99408 | Alcohol and/or substance abuse structured screening and brief intervention services, 15–30 minutes. | $33.41 |
| Commercial insurance, Medicaid | 99409 | Alcohol and/or substance abuse structured screening and brief intervention services, greater than 30 minutes. | $65.51 |
| Medicare | G0396 | Alcohol and/or substance abuse structured screening and brief intervention services, 15–30 minutes. | $36.25* |
| Medicare | G0397 | Alcohol and/or substance abuse structured screening and brief intervention services, greater than 30 minutes. | $71.42* |
| Medicare | G0442 | Screening for alcohol misuse in adults, 15 minutes. No coinsurance; no deductible for patient. | $18.30* |
| Medicare | G0443 | Brief face-to-face behavioral counseling for alcohol abuse, 15 minutes. Up to four per year for individuals who screen positive for alcohol misuse. No coinsurance; no deductible for patient. | $26.20* |
| Medicaid | H0049 | Alcohol and/or drug screening (code not widely used). | $24 |
| Medicaid | H0050 | Alcohol and/or drug service, brief intervention, per 15 minutes (code not widely used). | $48 |
Conclusion
Alcohol screening and brief intervention offers an evidence-based approach to helping your patients make healthier choices regarding their alcohol use. Moreover, this service is relatively easy to perform and readily billable for most payers. Why not start by prescreening a few of your patients today? For additional information, the Centers for Disease Control and Prevention has published guidelines for implementing alcohol screening in primary care, and the USAUDIT guide is available for primary care physicians.
