
With communities facing so much unrest, here are two skills you can apply to help promote healing.
Fam Pract Manag. 2021;28(1):23-26
Author disclosure: no relevant financial affiliations disclosed.

Family physicians lead by example and play a major role in the health and well-being of their communities. Their contributions go far beyond clinical care and are reflected in volunteer work on school boards, at homeless shelters, at free clinics, and within educational and service programs across the globe.
Community well-being is critically linked to individual well-being. Community health depends on the well-being of each member. Similarly, belonging to a strong community is essential to enhancing the well-being of individuals. It improves personal and professional health, and there's evidence it can reduce physician burnout.1,2
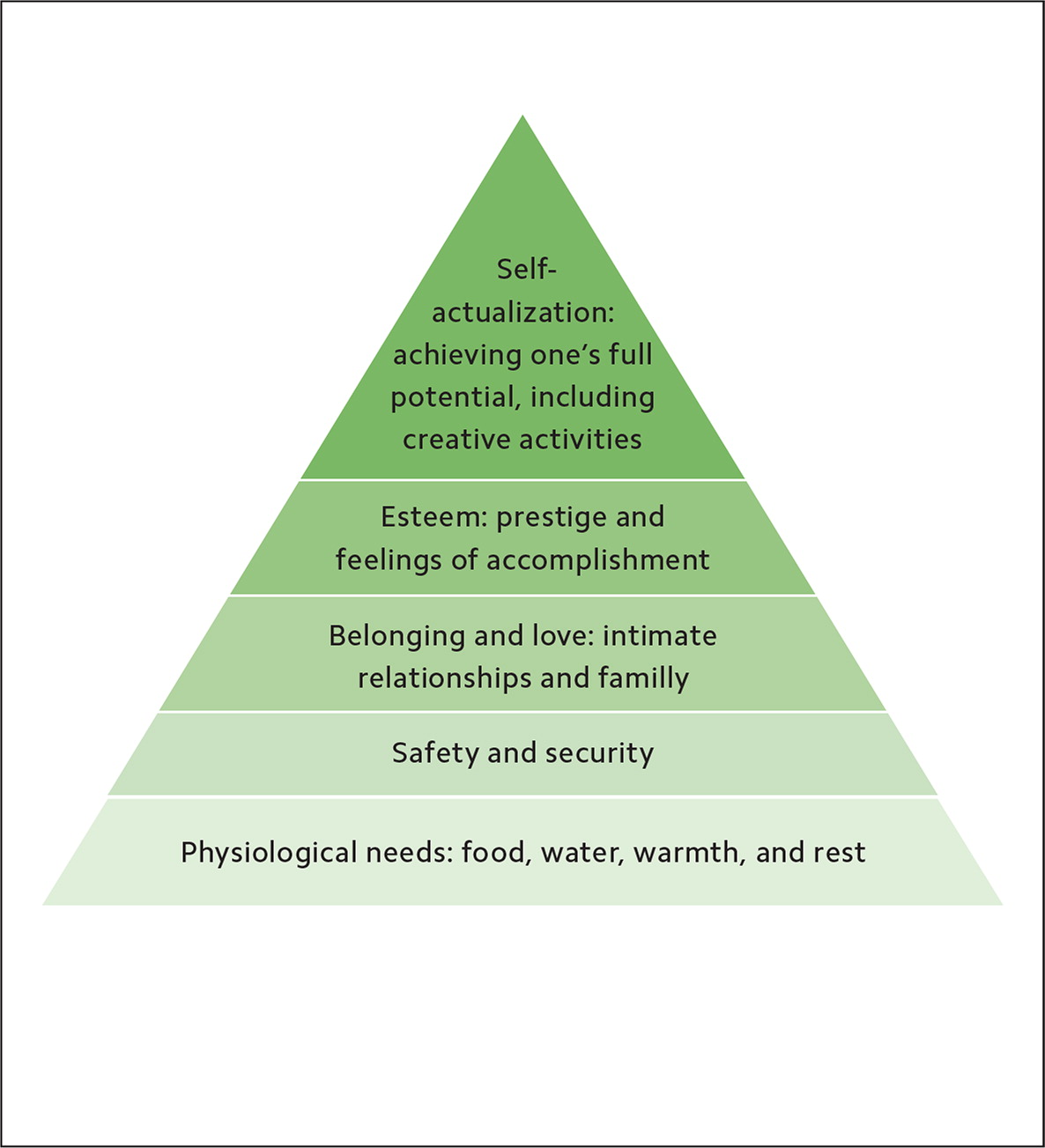
Maslow's Hierarchy of Needs suggests that reaching the highest level of achievement or self-actualization depends on a strong foundation. Physiologic needs (food, water, and rest) as well as the need for safety and belonging are primal and must be met before we can reach our full potential. Further, the overall health of a community depends on collective progress toward self-actualization.
The year 2020 will be remembered for the COVID-19 pandemic that turned our daily lives upside down, protests over racial inequities in American society, and political division. No community was immune from these ills, but some were hit harder than others. For example, the pandemic disproportionately harmed minority populations, with Black Americans experiencing death rates more than twice as high as white Americans.3
These challenges have shown us how small our world can be and how our well-being is linked across the globe. We win or lose together. When one member is unwell, oppressed, or silenced, the whole population suffers. Community well-being commands a unified and healthy population.
Building healthy communities requires excellent clinical care and attention to social determinants of health. It also requires incorporating two new skills into your practice: emotional intelligence and cognitive reframing.
KEY POINTS
Community well-being depends on the well-being of each individual, and a healthy community enhances the well-being of its members.
Adverse experiences result in negative thoughts, emotions, and actions, and have the capacity to diminish community well-being.
Family physicians can help build healthy communities and lead change by using emotional intelligence to resolve fear, and cognitive reframing to correct distorted thoughts.
EMOTIONAL INTELLIGENCE
Emotional intelligence is “a form of social intelligence that involves the ability to monitor one's own and others' emotions and to use this information to guide one's thinking and actions.”4 It involves three steps:
Acknowledge emotions. This is a challenging first step, as many of us have been trained to deny feelings. We often wear a superhuman badge, telling ourselves that things are “fine” no matter what we actually feel. We may think that we are too busy to stop and reflect on our emotions or those of others, and that it is easier and more efficient to just be “fine.” Over time, however, “fine” becomes draining, and emotional exhaustion settles in.
Labeling feelings can be achieved by asking ourselves, “What am I [or what is the other person] feeling?” This exercise may feel foreign at first. A helpful tool is the Mood Meter app, which can suggest a plethora of emotional adjectives — exhilarated, peeved, mellow, tranquil, sullen, morose, etc. Taking the time to acknowledge emotions and grant ourselves and others permission to feel them is ultimately healthier than trying to be superhuman and deny our emotions.
Understand emotions. Once we have acknowledged our emotions, we need to get to the root problem. Ask yourself, “Why am I [or why is the other person] feeling angry/frustrated/disappointed/etc.?” The “five whys” technique can help with root cause analysis. Here's an example:
Why is my patient feeling angry? He doesn't want to wear a face covering.
Why? He doesn't believe they work.
Why? He doesn't trust experts.
Why? He hates being told what to do.
Why? He fears having no autonomy.
This example shows that the root cause is often fear. Fear is a divisive emotion. It is also a natural part of human survival. Fear protects us from real danger but can also amplify negative reactions to perceived or exaggerated danger. When we feel afraid, our biology commands our sympathetic nervous system to “fight or flight.” We pay more attention, go on high alert, protect ourselves, and prepare to fight back. Understanding fear — what it stems from and how it influences our behavior — is critical to our well-being.
When fear exists within a community, “they” appear. They didn't wear a mask. They don't show respect. They don't observe the law. When “they” show up in conversations, an “us vs. them” mentality arises, which destroys trust. As fear grows in a community, so does division. As fear spreads in the health care setting, professional behaviors erode and health outcomes diminish.
Manage emotions. As we gain insight into the “why” and the fear behind negative emotions, we tap into each other's stories, which plants the seeds of empathy. We find out that “they” are not bad people, but people who have had bad experiences. We can then effectively manage our emotions, instead of just acting on them, and change our interactions.
COGNITIVE REFRAMING
Negative emotions and actions sometimes seem isolated, unwarranted, and sudden (appear out of nowhere), but they are often the result of distorted thoughts. Cognitive behavioral therapy, which grew from the work of Albert Ellis and Aaron T. Beck, focuses on shifting distorted thoughts to change negative emotions and maladaptive behaviors.5 This novel approach differs from previous methods that focused exclusively on changing behavior, and it has been effective in addressing dysfunctional thoughts that contribute to mental, physical, and emotional challenges.6,7
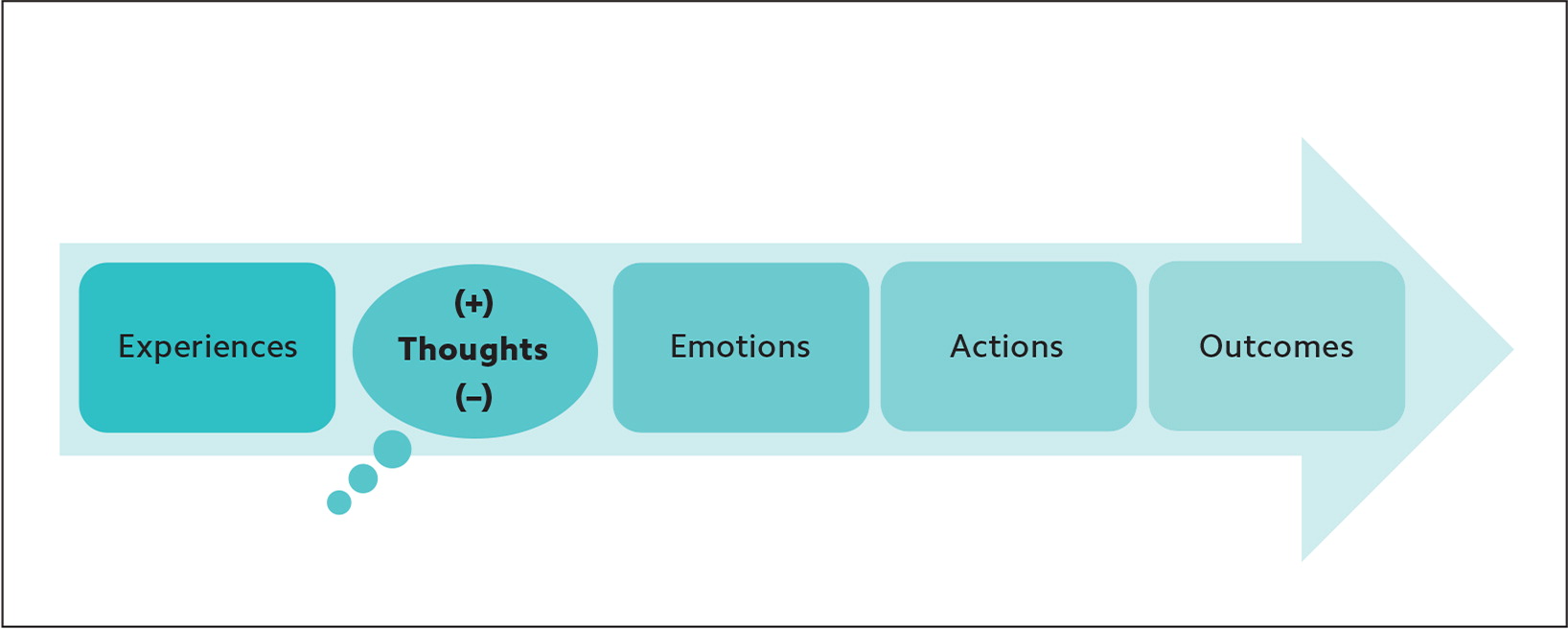
The “Thomas theorem,” the idea that what we believe becomes our reality, delineates the same tight connection between our experiences, thoughts, emotions, actions, and outcomes. (See “How thoughts influence outcomes.”) When our thoughts about an experience are negative, they will likely lead to negative emotions, actions, and outcomes; when our thoughts are positive, the reverse is often true. Adverse or harmful experiences elicit a “negativity bias,” meaning they ingrain stronger memories than positive or neutral experiences in order to maximize survival by helping us avoid future similar experiences.8,9 As a result, negative thoughts can reinforce negativity, eliciting destructive behavior and propelling negative emotions, actions, and outcomes.
There are 15 common cognitive distortions. While each of us has tendencies toward certain distortions, community-based stress is often caused by “emotional reasoning,” “blaming,” and “over-generalization.” Individuals feel certain that their negative experiences are the result of others' actions and respond with blame and condemnation, which becomes conviction.
| 1. Filtering: An exclusive focus on a single negative aspect of a situation. |
| 2. Polarized thinking: A belief that something is all good or all bad. |
| 3. Overgeneralization: A broad conclusion based on a single incident or unpleasant event. |
| 4. Jumping to conclusions: A hasty conclusion about someone's thoughts or behavior. |
| 5. Catastrophizing: An expectation that disaster has struck. |
| 6. Personalization: A belief that the individual alone is at fault for bad outcomes. |
| 7. Control fallacies: A sense that one is externally or internally controlled and helpless to fate. |
| 8. Fallacy of fairness: A resentment to being treated unfairly. |
| 9. Blaming: Holding other people responsible for our outcomes. |
| 10. Shoulds: A list of strict rules about how others should behave. |
| 11. Emotional reasoning: A conviction that what we feel must be true automatically. |
| 12. Fallacy of change: An expectation that others must change to meet our needs. |
| 13. Global labeling: Attachment of a generalized and unhealthy label to oneself or others. |
| 14. Always being right: An inability to see oneself as being wrong despite proof or damage to others. |
| 15. Heaven's reward fallacy: A belief that self-sacrifice and self-denial pay off. |
We can't erase history or deny the impact of negative experiences, but when our thinking about the past limits our effectiveness in the present, we must rethink the situation to provide a better future. Reframing allows us to interpret our experiences in more positive and productive ways. For example, our thoughts about the COVID-19 pandemic might be “This isn't fair. It's ruining my life.” This elicits emotions such as grief, fear, anger, and anxiety. Our actions might be to lash out at others and adopt an “us vs. them” mindset, which causes division. Reframing the experience opens the door for better outcomes. For example, we can choose to think “We are in this together. I am better off than some and can help others.” This reframing elicits gratefulness, optimism, and compassion, ultimately leading to unity and connection.
LEADING THE WAY
Building communities that are safe and healthy for all members of society is as challenging and rewarding as any work we will do in primary care. We succeed by walking the walk — facing fears, reframing thoughts, and sharing our stories with others. By keeping our own tanks full, supporting our families, prioritizing our teams, and serving as role models within our organizations, we lay the groundwork for healthy communities around the globe.
SERIES OVERVIEW
Creating your personal wellness plan (January/February 2020).
Self-care through mindfulness and strategies for promoting physical health (March/April 2020).
Family well-being through social connectivity and time management (May/June 2020).
Team well-being through conflict resolution and promotion of gratitude in the workplace (July/August 2020).
Organizational well-being through prioritizing purpose and creating resilient leaders (November/December 2020).
Community well-being through cognitive reframing and building emotional intelligence (this issue).
