
Am Fam Physician. 2022;105(3):281-288
Author disclosure: No relevant financial relationships.
Telemedicine can be useful for the management of diabetes mellitus. Remote monitoring of glucose levels improves A1C levels in people with poor glucose control. When multiple daily injections of insulin are required, continuous glucose monitoring improves glycemic control and increases patient satisfaction. Telemedicine diabetes prevention programs can be cost-effective. Teleretinal screening allows for the remote evaluation of retinal photos obtained at the primary care office to facilitate the timely completion of annual screening. Telemedicine for patients who have diabetes requires administrative and patient preparation before the visit. The physical examination should focus on the skin and extremities, especially the feet. Patients receiving telediabetes care require at least annual in-person visits for complete foot examinations, sensory screenings, and to address issues noted during previous telemedicine visits.
Telemedicine uses the electronic exchange of health information to improve a patient’s health and is classified into three categories. Synchronous telemedicine encompasses virtual care that is performed in real time. Asynchronous telemedicine involves acquiring medical data that are transmitted for assessment later. Remote monitoring is any health data continuously collected from the patient (e.g., remote blood pressure monitor, continuous glucose monitor). The use of telemedicine increased during the COVID-19 pandemic. The Veterans Health Administration was an early adopter to improve access to care and outcomes for a primarily rural population of veterans with multimorbidity, including diabetes mellitus.1
| Clinical recommendation | Evidence rating | Comments |
|---|---|---|
| Telemedicine should be used in addition to in-person visits to optimize glycemic control in patients with uncontrolled diabetes mellitus.2,19,20 | C | Consistent evidence from systematic reviews showing improvement in A1C levels |
| Continuous glucose monitoring can be helpful in patients who require insulin to reduce A1C levels, avoid hypoglycemia, and improve patient satisfaction.28–31 | C | Clinical review; disease-oriented studies evaluating glycemic control and hypoglycemia |
| Teleretinal screening should be considered in patients with diabetes as a cost-effective option for retinopathy screening in those who have access to this technology.43–45,48,49 | B | Consistent evidence from systematic reviews shows improved screening rates, cost effectiveness, and reduced rates of blindness |
Telemedicine used for the comprehensive management of diabetes (i.e., telediabetes care) has been shown to improve blood glucose control and some diabetes-related outcomes.2 Incorporating telemedicine into primary care can be challenging and requires an investment in staffing and training to establish the clinical workflows and workforce to care for patients remotely; however, it can improve the quality of care for patients with diabetes.2
Role of Telemedicine in Diabetes Care
The American Diabetes Association recommends improving care delivery at the systems level, offering self-management support, and using shared decision-making in the care of patients with diabetes.3 Telemedicine addresses these goals by increasing patient access to care through decreased travel requirements. It also improves outcomes by adding video visits and virtual nurse check-ins between physician visits, which improves diabetic glycemic outcomes.4 Remote monitoring allows the patient to communicate real-time blood glucose data to their physician to support diabetes self-management and recognize problems early. Telemedicine provides an opportunity to improve patient-centered approaches in diabetes care. In addition to eliminating the burden of travel, clinicians gain a glimpse into a patient’s living situation, which can facilitate discussions on food, housing, and economic security.
Medicare now pays for most telemedicine visits at the same rate as in-person visits for all types of telemedicine and patient locations.5 Private insurers have made similar accommodations.6 Medicaid and private insurer coverage of telehealth services is variable, and state Medicaid agency and insurance representatives can verify those policies. The future success of telediabetes care will depend on continued financial reimbursement and requires systemic solutions to overcome gaps in digital literacy.
Considerations for the Use of Telemedicine for Diabetes Care
Telemedicine poses challenges that require unique solutions in the care of patients with diabetes. Adaptations are required by the physician, ancillary staff, and health care organizations to ensure equitable and cost-effective care.
Office staff must be able to teach and troubleshoot telehealth technology. Relevant previsit information and home data about blood glucose levels and vital signs should be collected before the visit, which can offset the time saved from rooming patients and measuring their vital signs.
Plans for follow-up from the physician should be detailed and include the laboratory tests and measurements required before the next visit. Between visits, electronic messaging or telephone calls to the patient may be needed from nursing staff, diabetes educators, and office staff. Patients may require an in-person visit to address needs identified in a prior telemedicine visit.
The rapid increase in telemedicine use has revealed barriers to implementation.7 Internet limitations, especially in rural areas, can preclude the use of video technology. Telemedicine implementation could further isolate patients at high risk and exacerbate health care disparities. Physicians may struggle to use telemedicine if they lack resources for implementation and support (Table 17–16).
| Considerations | Challenges | Interventions | Evidence |
|---|---|---|---|
| Cultural competency | Telediabetes interventions are not universally applicable across cultures without modification | Communicate in the local language, involve indigenous health care workers, encourage community engagement, respect local cultures Use remote interpreter services | In one survey-based study, patients were equally satisfied with remote interpreter services and in-person interpretation8,9 |
| Digital literacy | Ability to use telemedicine can be affected by age and limiting comorbidities such as a visual or hearing impairment | Implement technical support and troubleshooting before, during, or after a visit Identify patients who are not good candidates for telemedicine | In one qualitative study, all age groups acknowledged independence and convenience as key benefits of diabetes care, but patients older than 50 years preferred in-person care10 |
| Physician practice setting | Telediabetes encounters may be difficult and time-consuming if technological issues arise during the visit | Screening for ability and willingness to use technology can be done by office staff before the visit and triaged accordingly | A survey of primary care physicians identified diabetes management as among the three most appropriate reasons for a video visit; factors that made telemedicine more difficult included poor cognitive function, non-English speakers, advanced age, and new patient visits7 |
| Psychosocial | Patients who have diabetes generally fare worse in measures of quality of life and emotional well-being | Telemedicine can support good physician-patient communication and trust, use of wearable diabetes technologies (continuous glucose monitors, insulin pumps), and disease-specific coping mechanisms | Smaller survey-based studies suggest a small improvement in quality of life and self-efficacy with the use of telemedicine11–13 |
| Systemic | Lack of telephone or internet access in rural areas and low socioeconomic status can lead to poor follow-up and difficulty using telediabetes care | Medicaid and Medi-Cal offer coverage or fee waivers for telemedicine consultation Veterans have access to programs that lend devices to patients to connect with clinicians14 Remote access stations and video-conference clinics can reduce travel time for patients without a home telephone or internet connection | A cohort study in 2020 identified lower use of telemedicine care among patients with lower household income and Latino and Black populations15 A systematic review of rural telemedicine interventions associated shorter travel distance and greater frequency of interventions with better glycemic outcomes16 |
Efforts to address these challenges are ongoing. The U.S. Department of Veterans Affairs ATLAS (Accessing Telehealth Through Local Area Stations) program partnered with organizations such as Walmart and the American Legion to establish telemedicine locations for patients without stable internet in their homes. There are 12 stations in the United States with plans to expand.17
Evidence for Telediabetes Care
GLYCEMIC CONTROL
Telemedicine has been implemented successfully in diverse subsets of populations with diabetes. Most of these studies demonstrate modest but clinically relevant improvements in glycemic control. One meta-analysis found a greater impact of telemedicine on type 2 diabetes than on type 1, which may be attributed to greater responsiveness to lifestyle modifications among patients with type 2 diabetes.2 Telehealth interventions have also been shown to be effective in Black and Latino patients despite systemic barriers to care.18
In a large systematic review of diabetes types and a heterogeneous mix of telemedicine modalities and interventions, telemedicine interventions led to a 0.6% reduction in A1C levels.19 Of all the telemedicine interventions, remote monitoring was found to be the most effective for telediabetes care. Remote monitoring uses text messaging or website portals to adjust medication doses based on glucose readings. Telephone calls were less effective, and telediabetes care did not affect quality of life, number of hypoglycemic episodes, or mortality.19
A recent umbrella review of telemedicine in type 2 diabetes also showed clinically relevant reductions in A1C levels.20 This average 0.5% change has been associated with fewer adverse cardiovascular outcomes.21 Increased frequency of interaction and younger patient age were associated with better glycemic improvement. A limited study of video vs. telephone modalities of telemedicine outside of diabetes care suggests that video improves diagnostic accuracy with equivalent outcomes overall.22
The benefit of telemedicine for diabetes care during pregnancy is uncertain. In a Cochrane review of pregnancies complicated by preexisting diabetes, telemedicine monitoring of blood glucose did not improve outcomes.23 These findings were similar to those of a previous meta-analysis that included pregnancies complicated by preexisting and gestational diabetes.24
However, telemedicine monitoring did improve outcomes for gestational diabetes in another recent large systematic review.25 More data are needed in this area.
REMOTE MONITORING
Remote monitoring uses telemedicine and additional human and technological support to gather and intervene on health data. Initial studies of remote monitoring involved a patient reporting self-monitored blood glucose to their physician to facilitate medication adjustment. Remote monitoring can include routine check-ins by a nurse, automated and interactive messaging, and direct telephone calls with physicians. In a meta-analysis of patients with type 2 diabetes, remote monitoring reduced A1C levels by 0.6%. Interventions varied, with some requiring frequent contact with staff.26 These interventions can be difficult to incorporate because they require patients to routinely log blood glucose levels via a secure platform and necessitate regular staff follow-up.
In the past decade, continuous glucose monitoring has become increasingly utilized for the remote monitoring of patients who are prescribed insulin. Continuous glucose monitoring measures interstitial fluid glucose and stores data trends in a cloud-based system. The analysis of glucose trends helps facilitate diet and insulin modifications without the need for frequent fingerstick measurements. Flash continuous glucose monitoring systems provide on-demand readings, whereas real-time continuous glucose monitoring systems measure glucose trends and alert the patient to impending hypoglycemia. Two new measures have been proposed to track glucose control and variability with continuous glucose monitoring. Time in range indicates the percentage of time in which the blood glucose level is at goal, and the glucose management indicator reflects average blood glucose measurements, analogous to an A1C level. These markers can be helpful in monitoring the status of a patient’s diabetes control, although they have not been shown to independently correlate with the same complications as A1C.
Current guidelines and reimbursement rules recommend continuous glucose monitoring for patients with diabetes who require multiple daily injections of insulin; continuous glucose monitoring in these patients is cost-effective.27 Continuous glucose monitoring decreases glucose variability, reduces hypoglycemic episodes, and improves satisfaction in these patients, although most studies have been industry funded.28–31
Continuous glucose monitoring can be implemented by primary care physicians and sustainably reimbursed.32 In type 2 diabetes, continuous glucose monitoring was found to slightly improve A1C levels over self-monitoring, with an average difference of 0.35% in a systematic review.33 Other outcomes, including body weight and blood pressure, did not improve. Further studies combining continuous glucose monitoring with other telemedicine interventions are needed to clarify the use of this technology in primary care.
NONGLYCEMIC OUTCOMES
Telemedicine interventions have some evidence of improving nonglycemic measures such as body weight and blood pressure by using the distribution of standardized scales and automated blood pressure monitors. These interventions have also been shown to improve health literacy and medication adherence.34
Telemedicine body weight outcomes are based primarily on people with prediabetes. The Diabetes Prevention Program, a clinically validated nutrition, weight loss, and physical activity program, has been adapted for use with telemedicine.35,36 The telemedicine-delivered program is now covered by Medicare.37 Weight loss from the telemedicine program is equivalent to that from in-person programs with significant cost savings.38 One study estimated a 25% reduction in diabetes incidence over five years and a more than $10,000 reduction in health care expenditures per person older than 10 years.39
Remote monitoring of blood pressure may be most valuable for patients at high risk, the underserved, and older populations.40 Improved blood pressure control through telemedicine use is attributed to lifestyle changes. In one small trial, daily monitoring of blood pressure resulted in improvement if patients with type 2 diabetes were also supplied with targeted lifestyle advice via a cellular telephone app.41 In a meta-analysis of nutrition counseling, patients with diabetes reduced their systolic blood pressure by 6 mm Hg with telemedicine compared with in-person counseling.42
TELERETINAL SCREENING
Retinal surveillance examinations can be completed using telemedicine. Asynchronous teleretinal imaging allows patients to be screened during routine appointments using a retinal camera that does not require pupillary dilation. Images are then sent to off-site eye-care specialists who can review and recommend follow-up for abnormal findings. Simulations conducted for U.S. government health systems suggest that teleretinal screening is more effective at reducing vision loss with a cost savings compared with in-person ophthalmology evaluations.43,44 Use of teleretinal screening has been shown to increase screening rates compared with traditional in-person visits.45 This technology provides convenience and reduces travel; however, it requires a clinic visit for completion. Patients with known retinopathy should have a follow-up with in-person examinations performed by an ophthalmologist. Because a retinal camera costs more than $15,000 and Medicare reimbursement is $64 per patient, teleretinal screening is more feasible for large health systems.46
The key benefit of teleretinal screening is improved adherence, which is important because only 62% of people with diabetes receive annual screening.47 Teleretinal screening can increase screening rates to 90% within one year.48,49 Ophthalmology guidelines recommend teleretinal screening as one option for screening.50
Practical Tips for Providing Telediabetes Care
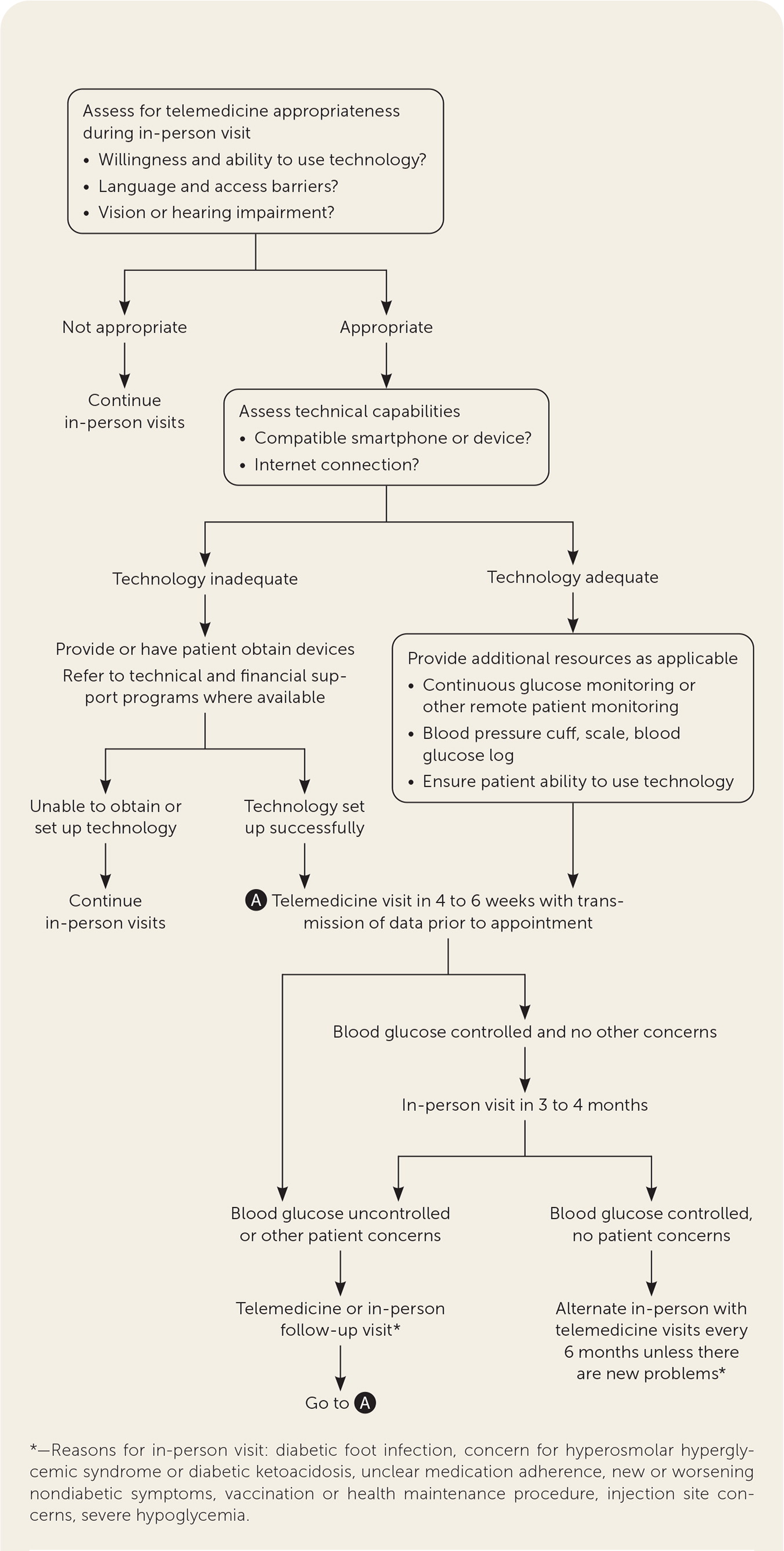
Before initiating telediabetes care, consider scheduling an in-person visit to establish baseline digital literacy and determine patient needs and appropriateness for virtual care follow-up (Figure 1). Patient preparation for virtual visits involves transmitting blood glucose logs, diet logs, and blood pressure and weight measurements for physician review. Digital health tools such as home scales, blood pressure cuffs, and continuous glucose monitors can help streamline the collection of these data. Continuous glucose monitoring can be tracked through manufacturer-supported cloud-based websites (e.g., Dexcom Clarity, Libreview) and third-party platforms (e.g., Glooko, Tidepool). Preparation requires administrative and patient time, which is partially offset by eliminating the office check-in process. Physicians may choose to optimize their clinic workflow by designating a specified number of clinic slots for telediabetes care.
A significant amount of relevant physical examination information can be gathered by video, and standardized patient-assisted virtual physical examination frameworks have been proposed.51 Important features of the telemedicine physical examination are listed in Table 2.52 The focused physical examination for diabetes care primarily involves the skin and extremities. Although complete foot examinations cannot be performed virtually, telemedicine evaluations were recommended by podiatrists during the COVID-19 pandemic.53,54 Any concerning findings should be confirmed with an in-person visit.
Preparing the patient (may be performed by clinical support staff)
|
Conducting the visit
|
Concluding the visit
|
Telemedicine provides clinicians with a unique opportunity to evaluate the home environment and any concerns with medication use. In-person evaluations of people with diabetes should occur at least annually for a complete foot examination with monofilament testing and retinal screening. Vaccinations and laboratory monitoring can be updated at these visits. Patients with poor blood glucose control or complications will need more frequent in-person care.
Data Sources: PubMed was searched using the key terms telediabetes alone and with telehealth, teleretinal, remote monitoring, outcomes, pregnancy, diabetes, and continuous glucose monitoring. The search included meta-analyses, randomized controlled trials, reviews, and editorials. Reference lists from the included meta-analyses were reviewed for potential sources. Search dates: September 10, 2020; October 15, 2020; February 5, 2021; and January 2022.
