FMX Content Hub
Replay key moments every day of the 2025 event and after.

FMX in Motion
The sessions are full, the conversations are flowing. Family medicine is life around here! Even if you couldn't make it this year, the FMX Content Hub shares great moments from the event.
Day in the Life at FMX
- David L. Tran, MD – Follow along as we experience a day at the AAFP’s COD and FMX.
- Eddie Needham, MD – A regular presenter at AAFP events, Needham presented two sessions at 2025.
Previously Published at FMX
- Push back and push family medicine forward, new AAFP president urges
- Suite of new physician leaders elected at 2025 Congress of Delegates
- Congress of Delegates adopts measures to strengthen physicians and patient health
FMX Public Relations
You didn't catch all the sessions you wanted to attend, so we selected a few each day to listen into and create quick takeaways for you! Sessions are available on FMX On Demand 24-28 hours after they run.
Don't forget: You receive 30 days of free FMX On Demand access with your FMX 2025 registration! That means if you missed something you wanted to attend onsite, you can easily rewatch it.
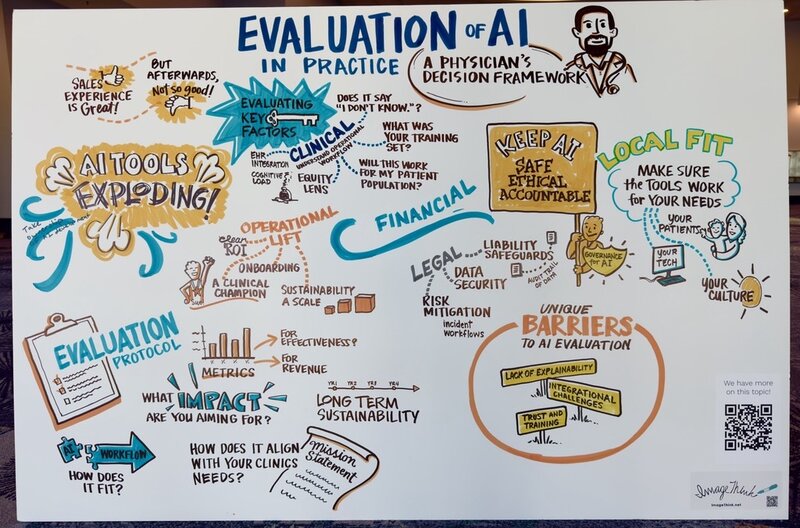
Evaluation of AI in Practice: A Physician’s Decision Framework
Why This Matters to Family Medicine
As AI tools rapidly enter clinical practice, family physicians need frameworks to evaluate which technologies truly serve their patients and practice. This presentation offers a practical, implementation-focused approach to navigating AI adoption—from scribes to population health tools—while maintaining the humanity at the heart of family medicine.
The speakers emphasize that AI evaluation isn't just about technical capabilities; it's about understanding how these tools fit into your unique practice environment, patient population, and payment model. Rather than being handed technology top-down, family physicians can take an active role in shaping how AI serves their practice.
Five Key Takeaways:
- Start Small, Learn Fast - Pilot with 5 clinicians maximum in one clinic for two months before scaling.
- Establish Baseline Metrics First - Measure current performance before implementation to track meaningful improvements
- Clinical + Operational + Financial + Legal + Local Fit - Evaluate all five dimensions, not just clinical benefits.
- Plan for Sunset - Have clear "no-go" criteria and rollback protocols before implementation.
- Continuous Monitoring Matters - Demo performance differs from real-world implementation; ongoing validation is essential.
Memorable Quote:
"How can we bring more humanity and connection to the care that we provide, and think about all the extra tabs we have open on our browsers and get rid of some of them with technology like AI?"
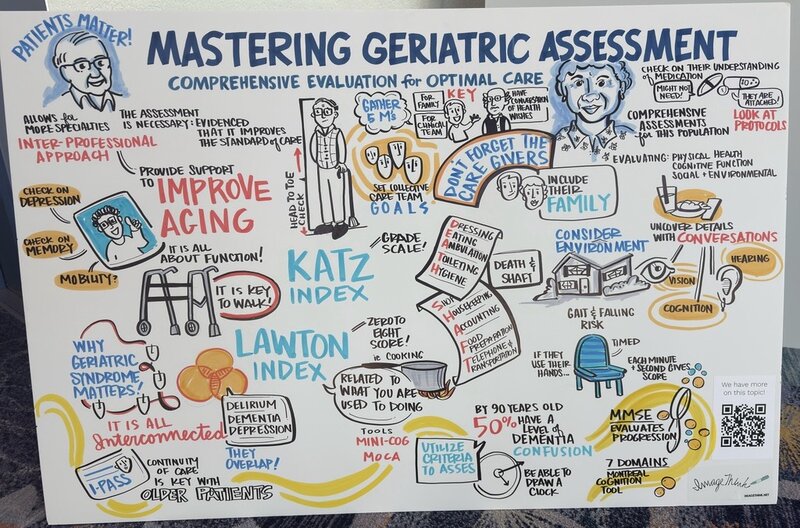
Mastering Geriatric Assessment: Comprehensive Evaluation for Optimal Care
Why This Matters to Family Medicine
As family physicians, we're on the front lines of caring for America's rapidly growing older adult population. This presentation on Comprehensive Geriatric Assessment (CGA) offers practical strategies to transform how we approach geriatric care—moving beyond treating single conditions to proactively supporting function and quality of life.
The evidence is clear: CGA improves outcomes by reducing hospitalizations, decreasing medication burden, and improving diagnostic accuracy. Yet in our busy practices, comprehensive assessment can feel overwhelming. This presentation addresses that challenge head-on, providing realistic tools and frameworks—like the "Five M's" (Mind, Mobility, Medications, Multi-complexity, and What Matters Most)—that make geriatric care manageable even in time-constrained visits.
What makes this approach truly family medicine is its emphasis on seeing the whole person in context: their home environment, caregivers, goals, and daily function. The presenters remind us that addressing geriatric syndromes isn't just good medicine—it's what allows our patients to stay home, maintain independence, and live according to their values.
Five Key Takeaways:
- Function is everything: "In the geriatric world, it's function, function, function"—functional status predicts outcomes better than individual diagnoses
- Talk TO patients, not about them: Direct conversation uncovers critical issues that charts miss.
- Mini-Cog takes 2 minutes: There’s no excuse not to screen cognition (three words: clock, drawing, recall)
- Deprescribing is prescribing: Use tools like deprescribing.org to systematically reduce medication burden.
- Support the caregiver: 80% are unpaid family members facing enormous burden—ask them "How are YOU doing?"
Memorable Quote:
"If someone doesn't know how to tell you their medications at the office, they probably don't know it at home."
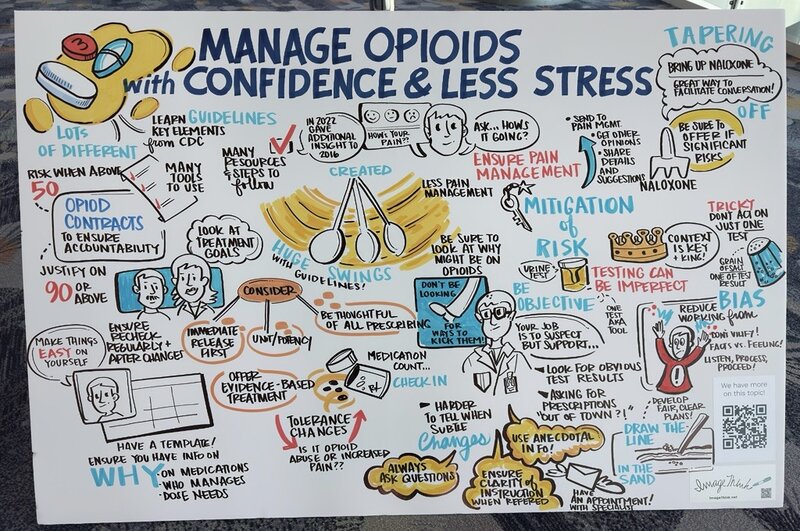
Manage Opioids with Confidence & Less Stress
Why This Matters to Family Medicine
In this FMX session, Dr. Radosh—a family physician turned addiction medicine specialist—provides practical, compassionate strategies for managing patients on chronic opioids.
This presentation matters deeply to family medicine because we're often the ones inheriting complex opioid cases, caught between patients' genuine pain and legitimate safety concerns. Dr. Radosh reframes the conversation: following CDC guidelines protects both you and your patients, while compassionate communication prevents the adversarial relationships that have become all too common. His approach centers on a crucial insight: "The patient's the one with the disease"—not you. When we remember this, opioid management becomes less about our anxiety and more about objective, guideline-based care.
Five Key Takeaways:
- Follow CDC Guidelines as Your Safety Net: Document why patients are on opioids, establish functional goals, and prescribe naloxone at ≥50 morphine equivalents or with risk factors.
- Use Your EMR Wisely: Create templates and smart phrases for opioid management—treat it like any other chronic disease.
- Ask the Magic Question: "What does the opioid do for you?" This simple inquiry reveals whether patients are using medications as intended.
- Medication Counts Matter: Random pill counts (not on first visits) help monitor adherence without being punitive.
- Unexpected Drug Screens Start Conversations: An abnormal result is the beginning of dialogue, not grounds for dismissal.
Memorable Quote:
“An unexpected drug screen is the start, not the end of a conversation."
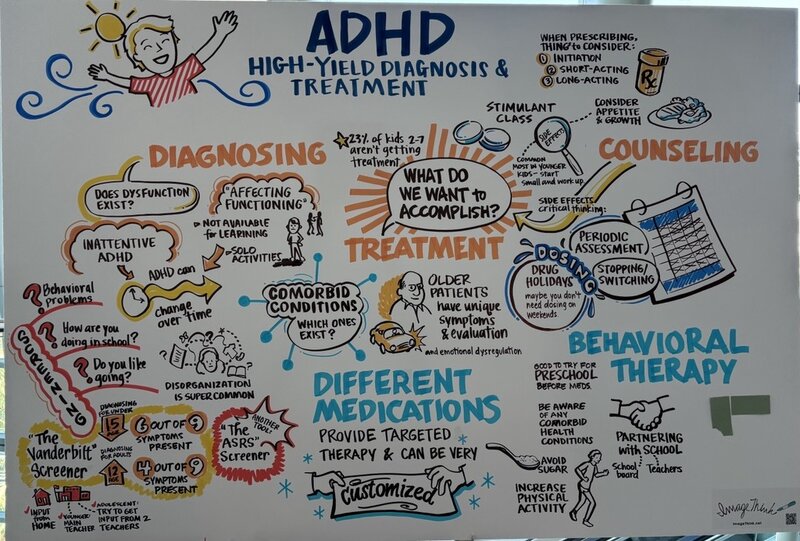
ADHD: High-Yield Diagnosis & Treatment
Why This Matters to Family Medicine
You may feel uncertain about ADHD diagnosis and treatment strategies. As primary care providers, we're uniquely positioned to identify, treat, and support patients with ADHD throughout their lives—from challenging elementary schoolers to struggling adults finally seeking answers. This practical, evidence-based session empowered family physicians to confidently diagnose and manage ADHD while recognizing when to treat comorbid conditions or refer for additional support.
Five Key Takeaways:
- Simplified Diagnostic Approach: Use the "quick cheat sheet" method—look for dysfunction in multiple settings, ask high-yield questions about school performance and completion of tasks, and utilize free screening tools like the Vanderbilt for children and ASRS for adults.
- Medication Management Made Practical: Start stimulants on weekends to observe side effects, dose after meals to minimize appetite suppression, and consider combining long-acting morning doses with short-acting afternoon doses for optimal coverage.
- Beyond Stimulants: Atomoxetine offers 70% effectiveness of stimulants without abuse potential, takes 4-6 weeks for full effect, and can be combined with stimulants or dosed at bedtime for chaotic morning routines.
- Adult ADHD Recognition: Symptoms must have been present before age 12 (not necessarily diagnosed), and diagnosis focuses on current dysfunction affecting work, relationships, or daily functioning.
- Holistic Treatment: Two-thirds of parents report medication helps, but nearly half found changing schools impactful—partner with schools for 504 plans, encourage physical activity before class, and address nutrition alongside pharmacotherapy.
Memorable Quote:
"I think we’ve really struggled with diagnosis. I think we’ve made things a little too complicated...so it’s important to take a step back. Use your skill set. Use your skill set and use your screeners to make sure you’re not missing anxiety, depression, bipolar."
Related AAFP content:
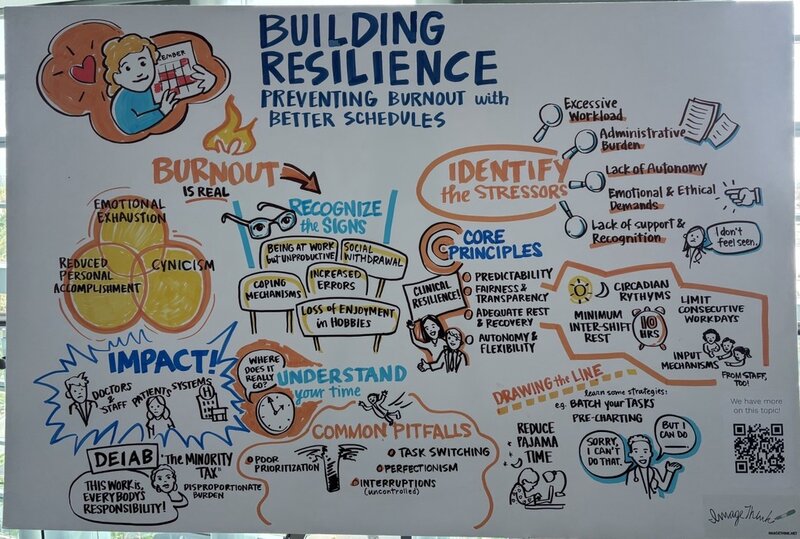
Building Resilience: Preventing Burnout with Better Schedules
Why This Matters to Family Medicine
Physician burnout isn't just about having a bad day—it's a systemic crisis affecting nearly half of all physicians, with profound implications for both clinician wellbeing and patient care. Dr. Amma Chaudhary guides attendees through the anatomy of burnout—emotional exhaustion, depersonalization, and reduced personal accomplishment—while offering practical tools for immediate implementation. Using real case studies, participants learn how to conduct their own time audits, identifying hidden time drains like excessive "pajama time" documentation and poorly structured meetings. The presentation moves beyond theory to actionable scheduling principles: protecting administrative time, implementing team-based care models, and establishing digital boundaries that preserve family time.
Five Key Takeaways:
- Track your time honestly using a weekly audit to identify where hours actually go—many physicians discover they're spending 20+ hours weekly on EHR tasks alone. Hint – there’s a guide in her slides.
- Protect 4+ hours weekly for dedicated administrative time to reduce after-hours "pajama time" documentation.
- Practice strategic "no" using direct, brief responses without lengthy explanations to protect your capacity.
- Batch similar tasks (emails, phone calls, charting) into focused time blocks rather than constantly task-switching.
- Implement the "two-minute rule" completing any task under two minutes immediately to prevent inbox buildup.
Memorable Quote:
“Burnout isn't just an individual physician problem—it directly impacts patient care, doubling the likelihood of patient safety incidents."
Related AAFP content:
Enhancing Communication Skills in Healthcare
Why This Matters to Family Medicine
Communication isn't just about exchanging information—it's the foundation of everything we do in family medicine. This presentation explores practical, evidence-based strategies to transform how we connect with patients, colleagues, and communities.
Here's what makes this crucial: 70-80% of serious medical errors stem from communication failures, yet when patients report good communication, they're 3-4 times more likely to adhere to treatment plans. We'll explore how mastering these skills reduces malpractice claims by 20-35% while building the long-term therapeutic relationships that make family medicine so rewarding.
Five Key Takeaways:
- Teach-Back Method: Have every patient repeat information in their own words—it significantly improves comprehension, reduces medication errors, and prevents readmissions.
- Health Literacy Matters: Design patient materials at 4th grade reading level or below, use plain language (say "blood thinner" not "anticoagulant"), and limit information to 2-4 key points.
- SBAR for Team Communication: Using this standardized tool reduces communication-related adverse events by 50%—literally one extra sentence of confirmation saves lives.
- Cultural Competence: 26 million Americans have limited English proficiency. Use professional interpreters, not family members, who misinterpret 50% of key information.
- Psychological Safety: Creating environments where team members feel safe speaking up prevents errors and strengthens collaboration—it's about valuing honesty over perfection.
Memorable Quote:
"Repeating back orders reduces communication-related adverse events by over 50%. That one extra sentence will reduce medical errors by 50%."
Related AAFP content:
Lifestyle Medicine for Prevention & Management of Diabetes
Why This Matters to Family Medicine
This session challenged conventional diabetes management and empowered family physicians to change the trajectory of their patients' health. Lifestyle medicine interventions can address the root causes of type 2 diabetes—not just manage symptoms. This isn't about adding more to your already full plate; it's about giving you practical, evidence-based tools that work in real-world settings, including FQHCs and underserved communities. You'll learn why "fiber should be your favorite F-word" and discover how simple dietary shifts, strategic exercise timing, and addressing the "ominous octet" of diabetes pathophysiology can produce remarkable results—like one patient who dropped their A1C from 8.5 to 5.9 through lifestyle changes alone, never even filling their metformin prescription.This session equips you to move beyond just prescribing medications and truly empower patients to take control of their health.
Five Key Takeaways:
- Insulin Resistance is a Fat Disease: While sugar plays a role, excessive dietary fat (especially saturated fat) accumulates in the liver, muscles, and pancreas, crowding out glucose and disrupting insulin signaling—this is the primary driver of insulin resistance.
- Fiber is the Missing Link: Most patients with type 2 diabetes are already eating plenty of protein, but they're fiber-deficient. High-fiber complex carbohydrates produce short-chain fatty acids that increase GLP-1 naturally, improve insulin sensitivity, and provide better glycemic control than protein-focused diets.
- Exercise Timing Matters: Exercise acts like insulin by increasing GLUT4 translocation to the cell membrane. Encourage patients to do light-to-moderate activity (even just walking) for 15-20 minutes after meals to significantly lower postprandial blood glucose.
- The Glycemic Load Advantage: Stop telling patients to avoid fruit. Use glycemic load (not just glycemic index) to guide recommendations—watermelon has a high GI of 72, but its typical portion yields a low glycemic load of 5 because it's mostly water and fiber.
- Address the "Ominous Octet": Type 2 diabetes involves eight pathophysiological defects (decreased insulin secretion, increased glucagon, hepatic glucose production, decreased muscle glucose uptake, increased lipolysis, decreased incretin effect, increased renal glucose reabsorption, and neurotransmitter dysfunction)—and lifestyle interventions can target every single one.
Memorable Quote:
"Even with our tons of medicines, the rates of diabetes is climbing. Why is that? We're not getting to the root cause of this disease."
Obesity Pharmacotherapy: Latest Advances & Insight
Why This Matters to Family Medicine
Obesity management is one of the most pressing challenges in family medicine today, affecting nearly every aspect of our patients' health—from diabetes and cardiovascular disease to mental wellbeing. This comprehensive session from FMX tackles the reality that while GLP-1 medications have revolutionized treatment, they're just one tool in our toolkit, and with coverage changes looming, we need to master the full spectrum of approaches.
We're on the front lines of the obesity epidemic, seeing patients struggle with weight-related comorbidities daily. With Medicaid planning to discontinue GLP-1 coverage in January 2026, family physicians need practical strategies that integrate medications with sustainable lifestyle interventions—approaches that work regardless of insurance coverage or formulary restrictions.
Five Key Takeaways:
- Start low, go slow with GLP-1s: Keep patients on the lowest effective dose (even 0.5 pounds/week loss counts). Rushing to maximum doses leaves nowhere to go when plateaus occur.
- Lifestyle first, always: Require 3-6 months of documented lifestyle interventions before medications. The foundation of sustainable change is behavioral, not pharmacological.
- Smart tapering prevents rebound: When discontinuing GLP-1s, taper extremely slowly—spacing doses to every other week, then monthly, rather than abrupt cessation which leads to 66% weight regain.
- Combination therapy breaks plateaus: When patients plateau on maximum GLP-1 doses, adding phentermine, topiramate, or naltrexone-bupropion can restart progress.
- Set realistic expectations with SMART goals: Work with patients to identify specific, measurable targets—like "plant-based dinners four nights weekly for six weeks"—rather than vague "lose weight" goals.
Memorable Quote:
"The medications that we use are meant to support lifestyle changes. It's not meant to be like 'give me that medication and just keep doing the same thing. Medications are adjuncts, not replacements.”

Anxiety Disorders in Adults
Why This Matters to Family Medicine
We all know that patient—the one who makes us feel anxious before we even walk in the room. This session tackles the real-world challenges of diagnosing and treating anxiety and panic disorders in your busy family medicine practice. You’re tapped for time, yet anxiety screening is now recommended for adults up to age 64. The good news? You can manage these conditions effectively without referring to psychiatry. This presentation offers realistic strategies to streamline screening, choose appropriate first-line treatments, and have those difficult conversations about benzodiazepines and substance use—all while maintaining the therapeutic relationship.
Five Key Takeaways:
- Empower your staff to administer screening tools (GAD-7, PHQ for panic disorder) before you enter the room—it saves time and reduces patient wait anxiety.
- SSRIs and SNRIs are first-line therapy for both generalized anxiety and panic disorders.
- Avoid benzodiazepines as first-line treatment. They increase risks of tolerance, withdrawal, and mortality without superior efficacy compared to antidepressants.
- Continue medication for at least 6-12 months to minimize relapse. Discontinuing before one year leads to up to 50% relapse rates.
- Address substance use directly. Caffeine, nicotine, alcohol, and cannabis often worsen anxiety despite patients believing they help. These require concurrent treatment for optimal outcomes.
Memorable Quote:
"I often see somebody in their 40s, but they've been this way all their life and they've probably met the criteria 20 years ago and just didn't get treatment."
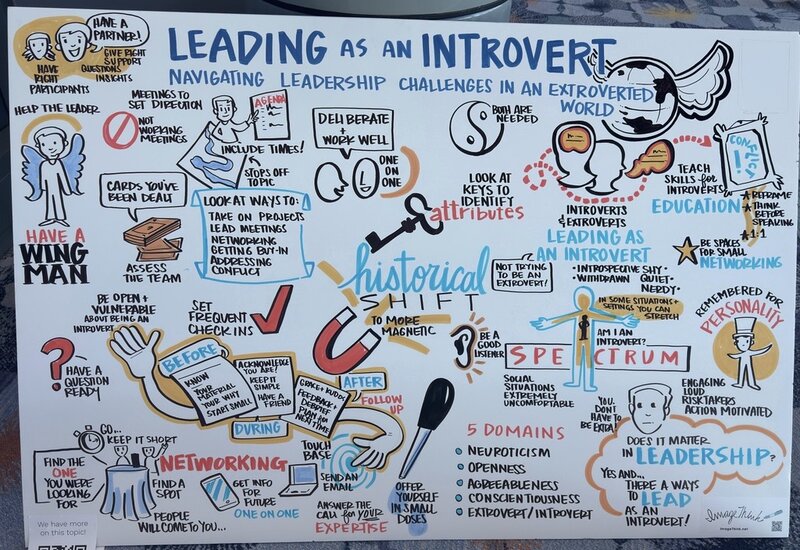
Leading as an Introvert: Navigating Leadership Challenges in an Extroverted World
Why This Matters to Family Medicine
Ever felt like leadership requires you to be the loudest voice in the room? This session challenged the "extroverted ideal" that dominates healthcare leadership, revealing how introverts bring unique and powerful strengths to family medicine. In Western culture, we've mistakenly equated effective leadership with being outgoing, risk-taking, and constantly "on." But the reality? Introverts possess exactly what modern healthcare needs: thoughtful listening, deep one-on-one connections, careful reflection before action, and the ability to create meaningful change without all the noise.
This presentation offers concrete tools for leading meetings effectively, navigating networking events without anxiety, securing buy-in for important initiatives, and addressing conflict with confidence. You don't need to pretend to be someone you're not to lead successfully.
Five Key Takeaways:
- Have a Wingman: Bring a trusted colleague (introverted or extroverted) to meetings, presentations, and networking events who can redirect conversations, ask planted questions, and provide backup when you need it.
- Master the Meeting Agenda: Create detailed agendas with time blocks and avoid "working meetings" where people wordsmith together—instead, assign individual work and reconvene to review progress.
- Leverage Introverted Networking: Skip the crowded room tactics and focus on one-on-one coffee meetings, thoughtful email follow-ups, and standing at a high-top table where people come to you instead of wandering around.
- Schedule Regular Check-ins: Put specific times on your calendar to follow up with team members—this structured approach works better for introverts than spontaneous "let's catch up sometime" conversations.
- Address Conflict with Your Strengths: Your ability to listen carefully, think before speaking, ask probing questions, and focus deeply makes you naturally skilled at resolving conflicts—lean into these abilities.
Memorable Quote:
"While we don't share small talk at all, we do like to have deep conversations with people. We work really well one-on-one and we're really intense in the things that we're passionate about, and those pieces can be incredibly important as you get through your own leadership journey."
Related AAFP content:
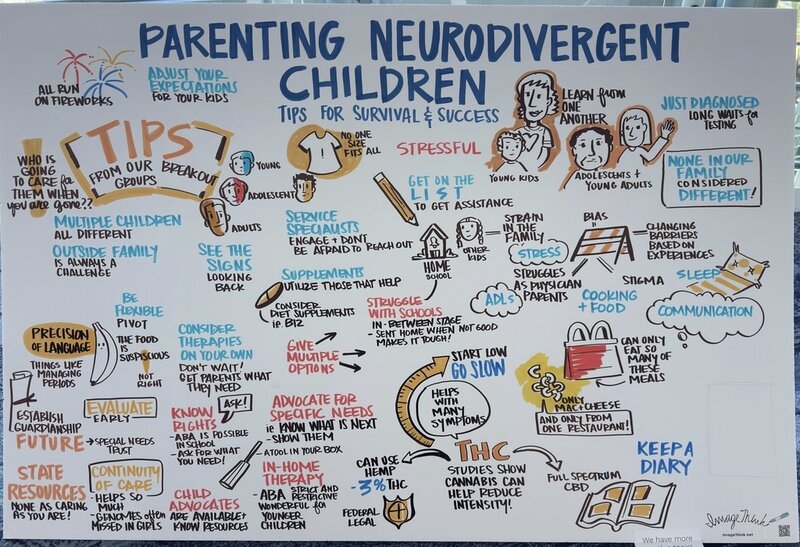
Parenting Neurodivergent Children: Tips for Survival & Success
Why This Matters to Family Medicine
Family physicians care for the whole family—but when it comes to our own neurodivergent children, we can feel lost navigating a system we thought we understood. This session brought together physician-parents to share the real experiences of raising children with autism, ADHD, and other neurodivergent conditions. This presentation broke down barriers physicians face when parenting neurodivergent children—from delayed diagnoses due to our own biases ("she's exactly like dad") to financial constraints despite having medical degrees. It emphasized that family physicians are uniquely positioned to support families through early identification, compassionate conversations about testing, and connecting families to resources before waitlists grow even longer.
Five Key Takeaways:
- Start referrals early—waitlists for diagnostic testing can now exceed six months.
- Girls often present differently and are often diagnosed much later than boys.
- CBD/cannabis may help with sleep, anxiety, and behavioral regulation in ASD.
- Educational advocates and IEP modifications are crucial—don't hesitate to use physician privilege.
- Special needs trusts can be established at any age and are protected from Medicaid recovery.
Memorable Quote:
"Physicians have difficulty with relationships, right? The stress of our profession can put strain on family. On top of that, the demand of parenting a neurodiverse kid can put a lot of strain on our relationships."
Related AAFP content:
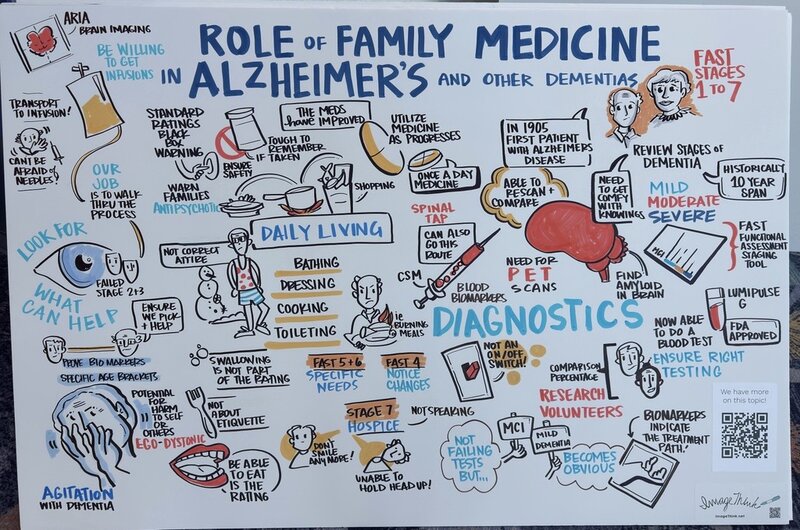
Role of Family Medicine in Alzheimer's & Other Dementias
Why This Matters to Family Medicine
As family physicians, we see more dementia than neurologists, just as we see more GERD than gastroenterologists and more depression than psychiatrists. This presentation equips you with practical tools to stage dementia using the FAST scoring system, understand when and how to use emerging blood biomarkers (finally—no more relying solely on clinical judgment that research shows is less than 50% accurate!), and identify which patients might benefit from the new anti-amyloid monoclonal antibodies. You'll learn to "cherry-pick" the right candidates—those fast 3 and 4 patients with MCI or mild dementia who can still walk and talk—and confidently guide them through discussions about IV infusions, biomarker testing, and realistic expectations. Plus, get clarity on treating agitation and psychosis.
Five Key Takeaways:
- FAST Staging is Essential: Learn to distinguish FAST 3 (MCI—aware of deficits, no functional impairment) from FAST 4 (mild dementia—obvious to others, IADL impairments) to identify candidates for anti-amyloid therapy. FAST 7 qualifies patients for hospice when language is lost.
- Blood Biomarkers Are Here: FDA-approved Lumipulse blood tests (spring 2024) make Alzheimer's screening accessible in primary care—finally, a practical alternative to PET scans and lumbar punctures with 91-97% sensitivity and specificity.
- Expand Your Alzheimer's Timeline: The disease doesn't start at diagnosis—we can now identify preclinical disease up to 15 years earlier through biomarkers, opening doors for prevention research and earlier intervention.
- Anti-Amyloid Therapy Requires Careful Selection: Lecanemab and donanemab are approved for MCI and mild dementia (ages 50-90 and 60-85 respectively) but require biomarker-positive confirmation, reliable transportation for infusions, and acceptance of cerebral edema/hemorrhage risks.
- Not All Psychosis Needs Treatment: Only treat delusions or hallucinations that cause harm to self or others (ego-dystonic). If the patient is comfortable with their experience (ego-syntonic), the risk of antipsychotic black box warnings outweighs benefits. When treatment is needed, quetiapine has the lowest adverse event frequency.
Memorable Quote:
“This isn't about becoming a dementia specialist—it's about embracing our role as the physicians who know our patients best and can shepherd them through this journey with competence and compassion.”
Related AAFP content:
Addressing Insomnia in a 24-hour World
Why This Matters to Family Medicine
Sleep is the foundation for health. As family physicians, we see the ripple effects of poor sleep daily: uncontrolled hypertension, persistent headaches, treatment-resistant depression, and accelerated cognitive decline. This presentation from Dr. Reddy, a family medicine physician who has spent 17 years in headache medicine, shares this approach: start with simple interventions that work for most patients, escalate thoughtfully when needed, and always keep your eye on helping patients become natural sleepers rather than medication-dependent ones. The real value here is learning to distinguish between process C (circadian rhythm) and process S (sleep drive) problems—a framework that transforms how you approach insomnia. You'll discover why that third of patients improve with sleep hygiene alone, why sleep restriction therapy works when nothing else does, and how to counsel patients on the real risks and limited benefits of sleep medications.
Five Key Takeaways:
- Ask the right question: Instead of "How are you doing?" ask "How well are you sleeping? Are you rested when you wake up?" You'll uncover issues patients won't volunteer.
- The 3P Model guides treatment: Identify Predisposing factors (migraine, anxiety), Precipitating events (job loss, divorce), and Perpetuating factors (poor sleep habits, medication dependence) to target interventions effectively.
- Sleep restriction therapy is your secret weapon: When 35% improve with sleep hygiene alone but 73% improve with hygiene plus sleep restriction, you need this tool. It consolidates fragmented sleep by temporarily limiting time in bed to match actual sleep time, building sleep drive.
- Know what you're prescribing: Z-drugs improve sleep latency by only 22 minutes on average and increase total sleep time by just 5%. One study showed taking even 18 pills per year increased cancer and death risk 3.5-fold. Use medications like training wheels—temporarily, while teaching better skills.
- Free resources exist: CBTI Coach (VA app), Michael Sealey's YouTube hypnosis videos, and online sleep diaries give patients tools without requiring referrals to sleep specialists most practices can't access anyway.
Memorable Quote:
"Sleep duration is linked to 7 of the 15 leading causes of death in the United States."
Breaking the Glass Ceiling: A Woman’s Road to Leadership
Why This Matters to Family Medicine
As family physicians, we champion comprehensive care for our patients. It's time we apply that same commitment to creating equitable pathways for women leaders in our specialty. Despite women comprising nearly half of family medicine graduates, they remain significantly underrepresented in leadership roles. From understanding implicit bias to mastering negotiation skills, this session equips you with actionable strategies to help you advance in your leadership journey—whether you're just starting out or years into practice.
Five Key Takeaways:
- Mentorship AND Sponsorship Matter - While mentors advise and guide, sponsors actively advocate for you in rooms where decisions are made. You need both.
- The STAR Method Works - Structure your accomplishments using Situation, Task, Action, Result (and Takeaway) to powerfully communicate your value during interviews and evaluations.
- Self-Advocacy Is Essential - Use the four P's: Power (know your worth), Presence (project confidence), Purpose (align your mission), and Permission (let go of internal biases).
- Utilize AAFP Resources - The Career Benchmark Dashboard and contract negotiation tools help you achieve pay equity and better working conditions.
- Organizational Change Is Possible - Advocate for transparent promotion pathways, implicit bias training, paid parental leave, and flexible leadership roles in your practice.
Memorable Quote:
"We can't do this alone. We need everyone to work together to be able to address the barriers. True progress requires allies—both women and men—working collectively to dismantle obstacles.”
Related AAFP content:
The One Big Beautiful Bill Act & What It Means for Your Student Loans
Why This Matters to Family Medicine
With the passage of the One Big Beautiful Bill Act, significant changes are reshaping federal student loan programs over the next three years. This session provides essential guidance on how these legislative changes will impact your repayment strategy, forgiveness eligibility, and long-term financial planning. Whether you're pursuing Public Service Loan Forgiveness at a nonprofit health center, managing high-interest Grad Plus loans, or considering refinancing options, understanding these policy shifts is crucial. Family medicine physicians often carry substantial debt while serving in community-based and underserved settings—making strategic loan management essential to financial wellness and career sustainability.
Five Key Takeaways:
- SAVE Plan Limbo: If you're currently on the SAVE plan, you've been in administrative forbearance since July 2024, and those months don't count toward forgiveness. Consider switching to Income-Based Repayment before July 2026 to maintain progress toward PSLF.
- New Repayment Landscape: Starting July 2026, only two repayment options will exist for new borrowers—a modified standard plan and the new RAP (Revised Affordability Plan), which extends IDR forgiveness from 20-25 years to 30 years.
- Grad Plus Elimination: Graduate Plus loans are being discontinued in 2026, capping graduate borrowing at $20,000 annually in unsubsidized loans—a major shift for medical education financing.
- PSLF Remains Protected: Both PSLF and Income-Driven Forgiveness are written into law by Congress and cannot be eliminated by executive order, though program requirements continue evolving.
- Refinancing Considerations: Current refinancing rates sit between 4-6.5%, making it worth evaluating every six months if you have private loans or aren't pursuing forgiveness—especially since there are no fees or prepayment penalties.
Memorable Quote:
"Both of those programs, PSLF and IDR forgiveness, they're both written in the law by Congress, so they can't just be evaporated off of an executive order."
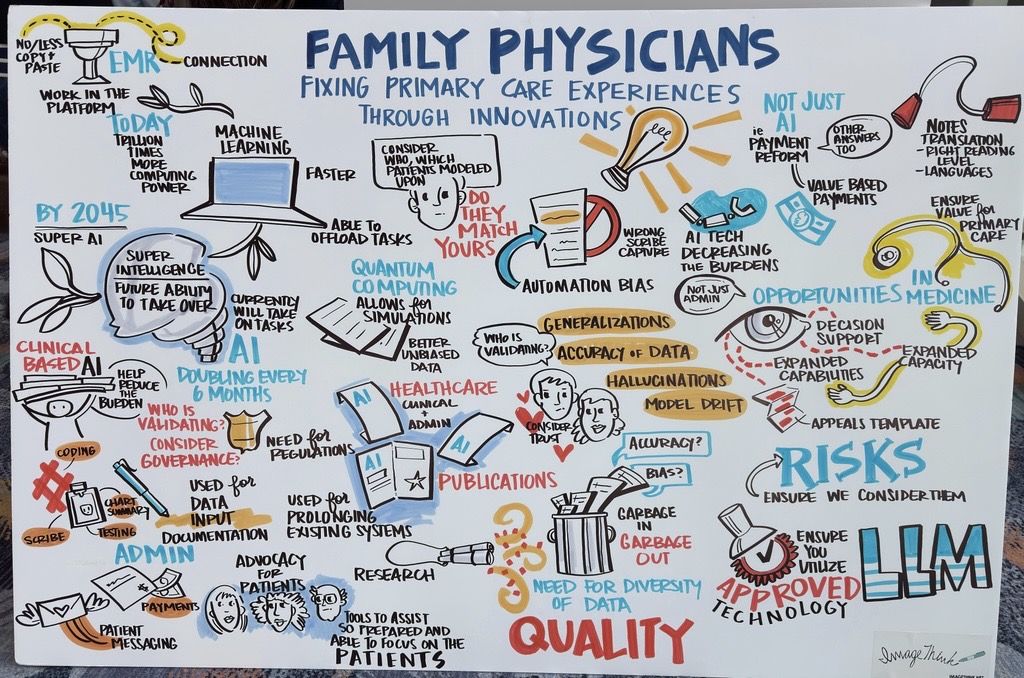
Physicians: Fixing Primary Care Experiences Through Innovations
Why This Matters to Family Medicine
This session explored how artificial intelligence is transforming family medicine—not as a silver bullet, but as a powerful tool to help physicians reclaim their calling. With AI capabilities doubling every six months, we're witnessing exponential growth that will reshape how we practice medicine. The discussion centered on practical AI applications already making a difference: ambient documentation that lets physicians look at patients instead of screens, intelligent inbox management that prioritizes and drafts responses, and clinical summaries that eliminate the "chart biopsy" before each visit. But the presenters emphasized that AI alone won't solve our problems—payment reform and appropriate staffing remain essential.
Five Key Takeaways:
- AI doubles in power every 6-7 months – What seems like a toy today will be magic in less than a year; a resident starting today will finish with AI 64 times more powerful
- Ambient documentation is the lowest-risk, highest-value use case – Physicians report reconnecting with patients, reducing documentation time from 12 minutes to 2 minutes per patient, and capturing complexity they previously missed
- Beware of "shadow AI" – Never put protected health information into unapproved AI tools without a Business Associate Agreement; even de-identified data can often be re-identified by large language models
- AI assistants can solve clinical problems, not just administrative ones – Next-generation inbox tools analyze the clinical decision needed, gather relevant data (last A1C, upcoming appointments), and suggest appropriate actions
- Value-based payment models amplify AI benefits – When combined with appropriate staffing ratios and clinical-first AI tools, physicians experience less burnout and more satisfaction
Memorable Quote:
"If we're not involved in this as family physicians, others are going to make our decisions for us, and we know that didn't really work out for us so far."
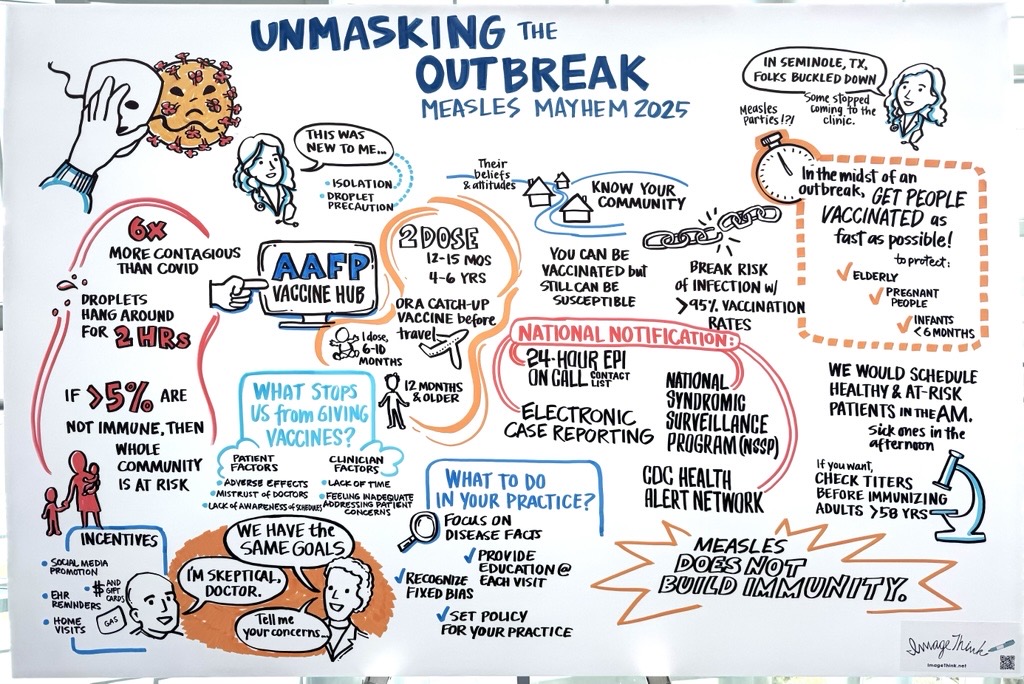
Unmasking the Outbreak: Measles Mayhem 2025
Why This Matters to Family Medicine
This session brings you to Ground Zero of a real measles outbreak in rural West Texas, where over 750 cases shattered the illusion that vaccine-preventable diseases are relics of the past. What started as one unvaccinated 8-year-old with a rash exploded into a community-wide crisis. The outbreak hit a perfect storm—low vaccination rates in Mennonite communities, deeply rooted vaccine hesitancy, and measles' extraordinary contagiousness (six times more infectious than COVID). You'll hear honest discussions about navigating vaccine hesitancy, building trust with hesitant families, and practical strategies that actually work. The presenters don't sugarcoat the challenges—from "measles parties" to vitamin A toxicity—but offer real solutions for your practice.
Five Key Takeaways:
- Measles is exceptionally contagious: Patients can transmit infection for 2 hours after leaving a room; one infected person can infect 12-18 susceptible contacts.
- Report immediately: Measles requires 24-hour notification to state health departments and CDC—know your epi-on-call number.
- Never repeat the series: If vaccination history is incomplete, continue from where they left off, never restart.
- Relationship matters most: Patients who refuse vaccines from staff often accept them when their trusted physician recommends them directly.
- Herd immunity threshold is 95%: We're currently at 90%, leaving communities vulnerable to outbreaks.
Memorable Quote:
"Keep the faith, hold to the science. This is just a period of time. We are the ones who have to keep the science for everyone."
We've shared stories that introduced you to some incredible family physician presenters over the years. Browse the list to see what you missed and when they’re speaking this year!
Ashley Wilk, MD
Family Doc Focus blog: FMX presenter has a passion for teaching peers
2025 FMX sessions: Worth a Shot: Understanding Current Vaccine Recommendations
Making Plant-Based Nutrition Easy Pea-sy!
Long-Acting Contraceptive (LARC) Workshop
Thomas Weida, MD
Family Doc Focus blog: Coding expert aims to help fellow family physicians get paid properly
2025 FMX session: Capture the Correct Evaluation & Management Outpatient Code
James Bigham, MD and Sanjay Batish, MD
AAFP Voices blog: Aiming for Safety: Prevent Firearm Injury With Open Patient Conversations
2025 FMX session: Firearm Injury Prevention: Practical Office Tips
Jason Domagalski, MD
AAFP Voices blog: Help patients understand their CRC risk, options for screening
2025 FMX sessions: The ABCs of LFTs
Improving Colorectal Cancer Screening & Management
Irritable Bowel Syndrome: Diagnosis & Effective Management
Jason Marker, MD
Family Doc Focus blog: FMX speaker played vital role in AAFP leadership programs
2025 FMX sessions: Leading as an Introvert: Navigating Leadership Challenges in an Extroverted World
(Panel) Navigating Your Career: Exploring Diverse Practice Models and Strategies for Success
Frank Domino, MD
FMX article: Domino Examines Past Year in Research, Looks Into the Future
2025 FMX session: Main Stage: Top 10 EBM Updates 2025
Lauren Brown-Berchtold, MD
Family Doc Focus blog: Physician Well-being Leader Driven to Help Peers
2025 FMX session: Empathy and Accessibility Virtual Reality Experience
Ecler Ercole Jaqua, MD
Family Doc Focus blog: FP Shares Expertise in Geriatrics and More
2025 FMX sessions: Navigating Incontinence: Urge, Instability and Overactive Bladder
Mastering Geriatric Assessment: Comprehensive Evaluation for Optimal Care
BLAST session - Lifestyle Medicine
Gender Affirming Care
Maya Bass, MD
Family Doc Focus blog: Chronic Conditions Forced FMX Presenter to Learn Resilience
2025 FMX sessions: Menopause Care for the PCP and Post Dobbs Primary Care Pearls
Inside Family Medicine: 100th Podcast Episode
Listen to Dr. Yalda Jabbarpour, Dr. Sarah Cole, Dr. Kate Tian, Dr. Kevin Wang, Dr. Jerry Abraham and Dr. Jen Caudle share their stories in Inspiring Journeys in Family Medicine. This episode celebrates the specialty's commitment to relationships and communities.

Taking the new Physician’s Journey Quiz will help you build a personalized FMX! In just a few minutes, you’ll uncover your learning style. You can use that style to:
- Find sessions that fit your interests
- Make connections that energize you

The FMX Mobile App
Your guide to everything at FMX!
- Plan your agenda each day and search for specific topics
- Find and chat with other FMX attendees
- Use maps to find your way around

Family Medicine Week
Thanks for celebrating Family Medicine Week with us! By sharing your story, you will:
- Help highlight the trust at the heart of family medicine
Collected stories will be shared in future campaigns to show their lasting impact.
